This information is for people with Ulcerative Colitis who are taking etrasimod, also known as Velsipity. It is also for anyone who is thinking about starting treatment with etrasimod. Our information can help you to decide if this treatment is right for you. It looks at:
- How the medicine works
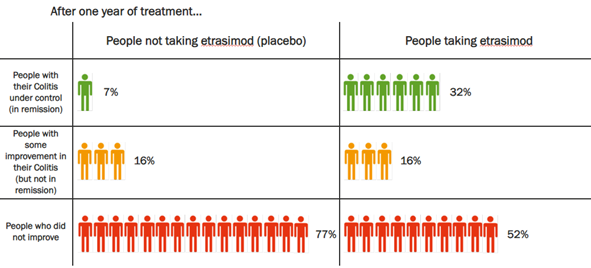
- What you can expect from the treatment
- Possible side effects
- Stopping or changing treatment
This information might use words you have not heard before. Our page on medical words can help provide an explanation.
This information should not replace advice from your healthcare professional. Talk to your IBD team or read the leaflet that comes with your medicine for more details. You can also find out about your medicine at medicines.org.uk.
Etrasimod is not currently recommended for people with other forms of Inflammatory Bowel Disease, such as Crohn’s Disease or Microscopic Colitis. Where we use the term ‘Colitis’ in this information we are referring to Ulcerative Colitis.