How you take steroids will depend on how severe your Crohn’s or Colitis is, and which part of your gut is affected.
Oral steroids
These are steroid tablets, capsules, granules, dissolvable tablets or solutions that you swallow. The patient information leaflet that comes with your steroids will tell you how to take them. You will usually take oral steroids in the morning. You should take them with or just after food. Taking oral steroids in the morning can help reduce side effects.
The instructions may be different for delayed-released oral steroids. This includes budesonide or beclomethasone dipropionate (Clipper). You may need to take these before food in the morning. It’s important to swallow these medicines whole and not to chew, crush or break them. This may stop them from working.
Intravenous (IV) steroids
This is an injection or infusion of a steroids into a vein. Intravenous steroids are used for severe flare-ups and can give the quickest response. You would only have intravenous steroids in hospital. You may then switch to oral steroids.
Rectal steroids
These are steroids that you insert into your bottom (rectum) with an enema or suppository. Enemas are liquids or foams, which you insert into your bottom with an applicator. Suppositories are small bullet-shaped capsules of medicine, which you place inside your bottom.
Read the instructions that come with your steroids. They’ll explain the best way to use them and often have pictures to help. In general:
- Insert foam enemas into your bottom while standing up, with one leg raised on a chair.
- Insert liquid enemas while lying down on one side. You’ll need to stay lying down for several minutes to give it time to work.
- Gently insert suppositories into your bottom and allow them to dissolve.
Do not worry if you do not quite get it right the first few times, or if you spill some. It’ll soon become another part of your routine. If you are having difficulty using your medicine, talk to your IBD team.



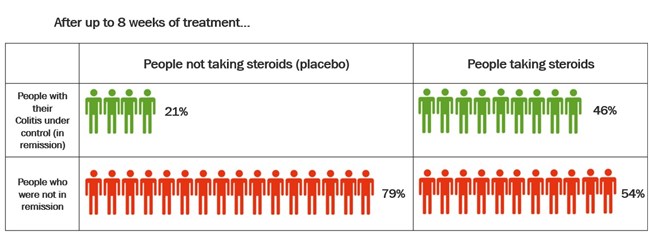
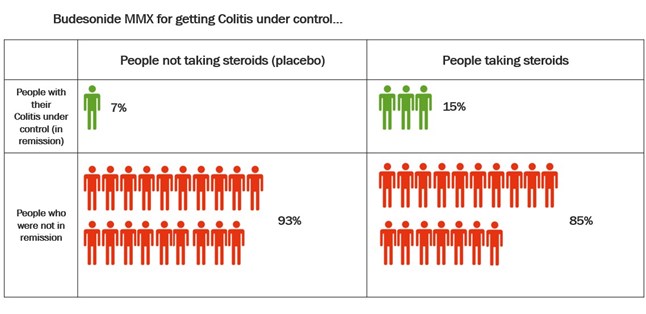
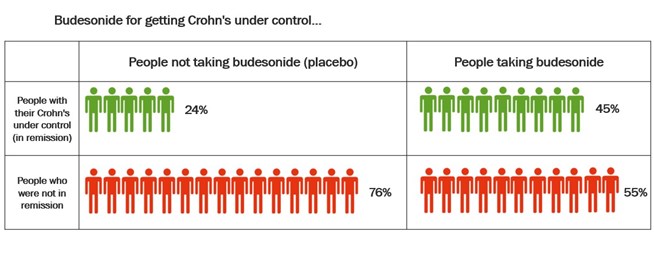 Studies have also compared budesonide MMX with placebo in the treatment of Ulcerative Colitis. Budesonide-MMX designed so that the budesonide is not released until it reaches the colon. This means it can be useful in the treatment of Colitis. The table below shows the results of these studies.
Studies have also compared budesonide MMX with placebo in the treatment of Ulcerative Colitis. Budesonide-MMX designed so that the budesonide is not released until it reaches the colon. This means it can be useful in the treatment of Colitis. The table below shows the results of these studies.