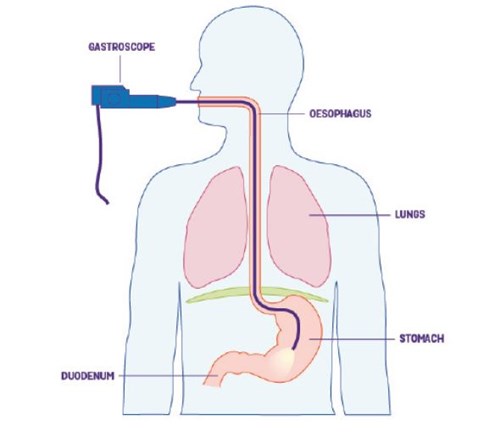
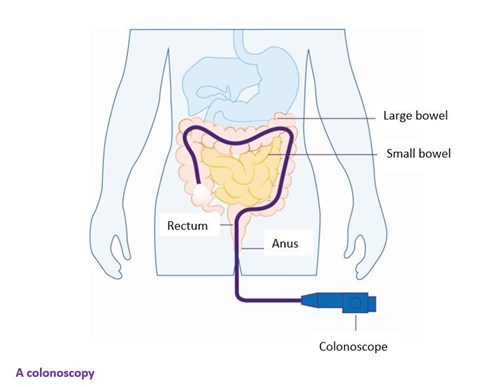
You can’t be diagnosed with Crohn’s or Colitis from just one test. Your doctor will need to gather lots of information to find out why you’re unwell. This can sometimes take time but it’s important you get the right diagnosis. The symptoms of Crohn’s and Colitis may be like other conditions, such as irritable bowel syndrome (IBS). To help understand what’s going on in your body, your GP will consider all your symptoms, together with some early investigations. These might include an examination of your tummy, as well as tests on your blood and poo. Your GP may also send you to have endoscopies, scans or X-rays. These are all tests to look inside your body.
Physical examination
Your GP might examine your tummy (abdomen) area to check for any lumps or to see if it’s tender. They may also check your bottom for piles, also known as haemorrhoids. You can request a doctor who’s the same sex as you, or you can ask for a chaperone for your examination. A chaperone is someone who can go with you to your examination and is usually the same sex as you, is impartial and does not know you.
Blood tests
Blood tests can show several different things. They can be used to see if you have inflammation in your body. They can also show if you’re low in iron, known as anaemia, or if you lack certain vitamins. Anaemia could suggest that you’re not absorbing the right nutrients or that you have small amounts of bleeding somewhere in your gut. These are both common in Crohn’s and Colitis. Your GP can also order a special blood test to check for signs of Coeliac disease. Coeliac disease is an immune condition that becomes worse when you eat foods that contain gluten. The symptoms of Coeliac disease can be like the symptoms of Crohn’s and Colitis. You can take Coeliac UK's online assessment to see if you should be tested for the condition.
Tell the doctor or nurse before your test if you’re worried about needles or seeing blood. They can make sure you’re as comfortable as possible and answer any questions you have.
Stool (poo) tests
Your poo might be tested for signs of bleeding or inflammation. It may also be checked for infections, like a Clostridium difficile infection, often known as C.Diff. For these tests, also called stool or faecal tests, you’ll need to collect a sample of your poo in a clean, dry screw-top container. Your doctor will give you this container and let you know what to do with it. You can find out more on how to collect and store a poo sample on the NHS website.
The thought of needing to give a sample of poo can be off-putting. But these sorts of tests are incredibly useful. They can help with your diagnosis, which means that you get the right sort of treatment for you.
Faecal calprotectin tests
Your GP may arrange for your poo to be tested for something called faecal calprotectin. Faecal calprotectin tests can show if there’s inflammation in your gut. This can be a sign that you may have Crohn’s or Colitis. However, a high faecal calprotectin result can also be caused by other issues, such as diarrhoea from an infection, gastroenteritis or certain types of cancerous and non-cancerous tumours.
Usually, levels that are above 100ug/g (micrograms of calprotectin per gram of poo) are considered to be a raised level. Higher levels may suggest that you should have further tests for Crohn's or Colitis. Not all hospitals and clinics use the same cut-off point of 100ug/g.
Lower levels of faecal calprotectin could indicate that you have irritable bowel syndrome or another non-inflammatory condition. However, lower levels can’t completely rule out Crohn’s or Colitis. You may have a repeat test after 6 weeks if your symptoms carry on.
A faecal calprotectin test may not be helpful for diagnosing Microscopic Colitis. For this condition, faecal calprotectin levels are often quite low.
Faecal calprotectin tests in children
Just like adults, faecal calprotectin tests are sometimes used to help diagnose Crohn’s or Colitis in children and young people aged under 18. See above for more information.
A child’s calprotectin levels may be assessed by a specialist in a hospital or clinic, rather than a GP.
There are no agreed cut-off levels that reliably show inflammation in children. Sometimes, the same faecal calprotectin cut-off levels as an adult might be used in children over four. But these will be used cautiously.
Children’s levels of calprotectin may be naturally higher than an adult’s and can vary. This can make it difficult to interpret, particularly in children younger than six.
To help with diagnosis, these tests may be used alongside a list of the child’s symptoms. Using both can help give a full picture of what’s going on.
Faecal immunochemical test (FIT)
Generally, if you’re older than 60, your GP may not use the faecal calprotectin test. This is because they may want to rule out other conditions, such as bowel cancer. Some hospitals and clinics may not use the faecal calprotectin test for some people with certain symptoms under 60 years old.
Your GP might use a FIT or faecal immunochemical test instead. This can check for small amounts of blood in your poo. Blood in the poo does not always mean a person has cancer. A FIT test may show blood in your poo due to something else, such as Crohn’s or Colitis.



 Become a member: Find out about the benefits of joining our amazing community
Become a member: Find out about the benefits of joining our amazing community
