Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last full review: November 2024
Next review date: November 2027
If your child has been diagnosed with Crohn’s or Colitis, it’s natural to feel worried about what this could mean for them and your family. But there’s lots you can do to help your child live life to the fullest.
This information looks at:
The information is aimed at parents of children under 16, but a lot will still be relevant if your child is older.
This information might use words you have not heard before. Our page on medical words can help provide an explanation.

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Crohn’s and Colitis are the two main types of Inflammatory Bowel Disease (IBD). They are not the same as Irritable Bowel Syndrome (IBS).
It’s important to look after yourself as well as your child. You can get support from your child’s IBD team, friends and family, other parents in a similar situation, and from Crohn’s & Colitis UK.
Finding out your child has Crohn’s or Colitis can cause a range of emotions. But you’re not alone. More than 500,000 people in the UK, about 1 in 123 people, have Crohn’s or Colitis. Almost 1 in 5 people with the condition are thought to be diagnosed before the age of 18. This means there are thousands of other parents in a similar situation, with similar experiences and concerns.
Crohn’s and Colitis are lifelong conditions. There is no cure, but there are treatments available to help keep symptoms under control. Many of your child’s symptoms should improve after they start treatment.
Crohn’s and Colitis affect everyone differently, and symptoms can change from one day to the next. Some children will take medicines, while other children may need surgery.
Crohn’s and Colitis are unpredictable. Your child will likely have periods of good health, known as remission. At these times, they may have no symptoms at all. But there will probably be times when their condition makes them feel unwell. These times are known as flare-ups, relapse or active disease. Treatment aims to control your child’s symptoms and help them stay in remission.
Most children with Crohn’s or Colitis continue to go to school and take part in sports and other interests. They can go on to further education, work, have a family of their own and enjoy life.
Your child’s journey through life may not be what you expected, but children are very resilient. Most cope very well with their condition. Your child may have to slow down or take a break at times. But many children tell us that their condition does not stop them from doing the things they love.
Being diagnosed hasn’t stopped me or changed my life much. I still train six hours a week with my gymnastics team and compete regularly. Life becomes a bit different but it’s really just about remembering to do a few more things, like taking your medication.
Rosie
Living with Crohn's
Coming to terms with your child’s diagnosis can take time for you and your family. Everyone copes differently and there is no right or wrong way of doing or feeling about things.
Many parents feel guilty or even blame themselves for their child’s condition. But we do not know what causes Crohn’s or Colitis, so there’s nothing you could have done differently to prevent it.
It’s easy to think ‘is it my fault in some way? Could I have done something to prevent this from happening?’ The truth is that no you couldn’t and no it’s not your fault.
Lee
Parent of Sam, living with Crohn's
It’s common to need time to adjust as you get used to everything. You may feel overwhelmed and out of your depth at first. Try to remember that you are not on your own. There is lots of support out there for you, including:
Find out more in the section support for you.
It’s important to look after your own emotional and physical health, even if it’s hard to find the time. Try to find something that works for you. This might include taking a walk, practising mindfulness, or simply spending time with a loved one. If you do not want to leave your child with anyone else, you could invite friends to your house instead of going out.
Try to ask family and friends for help if you can. This could include support with medical appointments, or times when you need a break. There may be people who care about you and want to help, but do not know how.
I do take it all on myself because there's so many dots to join up. The treatment, getting the drugs, making sure you’ve got appointments, dealing with the school. But when I can, I try and get out and have a long walk and just kind of clear my head on my own.
Stuart
Parent of Charlie, living with Crohn's
Crohn’s Disease and Ulcerative Colitis are two types of Inflammatory Bowel Disease (IBD). They cause painful ulcers and inflammation in the gut.
The inflammation in Crohn’s and Colitis affects how your body digests food, takes in nutrients and gets rid of poo. Crohn’s and Colitis can be diagnosed at any age, but they are less common in very young children and babies. Crohn’s and Colitis are lifelong conditions.
IBD is not the same as IBS, which stands for Irritable Bowel Syndrome. IBS has some similar symptoms but is a different condition and is treated differently. The NHS website has more information on IBS.
The gut is the part of your body that takes food and nutrients in and carries poo out. The gut starts at your mouth and ends at your bottom, known as your anus.
Crohn’s can affect any part of the gut, from mouth to bottom. It’s most common in the small bowel and colon. The areas of inflammation are often patchy, with sections of normal gut in between.
The walls of your bowel have layers. The inner layers take in nutrients from food, and the outer layers help move food through the gut and waste out of the body. Crohn’s can affect all layers of the bowel wall.
‘Crohn’s Colitis’ is a type of Crohn’s Disease where only the colon is inflamed. This is because ‘colitis’ means inflammation of the colon. It does not mean your child has both Crohn’s Disease and Ulcerative Colitis.
Ulcerative Colitis is inflammation and ulcers in the rectum and colon, which are two parts of the large bowel. In Ulcerative Colitis, only the inner lining of the bowel wall is affected. When we say Colitis in this information, we mean Ulcerative Colitis.
Microscopic Colitis is also inflammation of the colon. But unlike Ulcerative Colitis, Microscopic Colitis does not cause ulcers, and there is no blood in the poo. Only the inner lining of the bowel wall is affected. Doctors have to use a microscope to see the inflammation.
Microscopic Colitis is usually found in people over the age of 50, but it can occasionally affect children.
For more information visit our information on Microscopic Colitis.
Inflammatory Bowel Disease Unclassified, shortened to IBDU, is sometimes known as Indeterminate Colitis. If your child is diagnosed with IBDU, they have features of both Crohn’s and Colitis. As your child grows older their condition may change and start to look more like one condition than the other. If this happens, their diagnosis may be revisited and changed from IBDU to either Crohn’s or Colitis.
The charity CICRA has more information about IBDU in children.
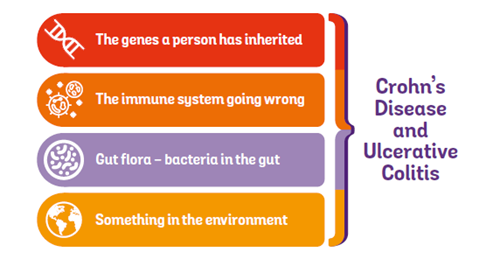
The exact cause of Crohn’s and Colitis is not known. But there are several things that may play a role, including:
Most people who have Crohn's or Colitis in their family will not develop either condition. But your risk is higher if a close family member is affected. It’s difficult to know what the exact risk might be, but research estimates that:
A child could develop either condition, but they’re more likely to develop the same condition as their family member.
It is possible for more than one child in a family to develop Crohn’s or Colitis. We do not know the exact risk, and most children who have a brother or sister with Crohn’s or Colitis will still not develop either condition.
Speak to your child’s IBD team if you have another child with symptoms.
The next section looks at symptoms of Crohn’s and Colitis. Everyone experiences Crohn’s and Colitis differently. There’s no way to know which symptoms your child might get. Or how they might be affected by these symptoms. But it can be useful to know what to look out for.
When your child is having a flare-up, they may experience:
Albert was pale, tired and had a very sore bottom. He was emptying his bowel a lot, and his poo sometimes had blood and mucus in it.
Sarah
Parent of Albert, living with Colitis
Crohn’s and Colitis do not just affect the gut. Both conditions can cause problems in other parts of the body too. You might hear these called extra-intestinal manifestations, or EIMs. You may notice some of these before your child has any symptoms in their gut.
Children with Crohn’s or Colitis may grow more slowly or not grow as well as other children. They may start puberty later or have weaker bones. This can be caused by lots of things, including:
Your child’s IBD team will consider their growth when planning treatment options with you. The aim is to manage your child’s condition, while also helping them to grow and develop as normal. Talk to your child’s doctor if you have any concerns about this.
Your child might have swelling, pain or stiffness in their joints, known as arthritis or arthralgia. Treatment for your child’s Crohn’s or Colitis can help with this. See our information on joints for more.
Some children get mouth ulcers, sore gums, swollen lips or cracks in the corners of their mouth. This is more common in children with Crohn’s and is sometimes called oral Crohn’s.
Treatment for your child’s Crohn’s or Colitis should help with this. Their IBD team may also prescribe a medicated cream, gel or mouthwash. Take your child for regular dental check-ups, as their dentist may also be able to give advice on mouth problems.
There’s some evidence that avoiding cinnamon and benzoates, which are found in some processed foods and fizzy drinks, may help. Ask your child’s IBD team for a referral to a dietitian before changing your child’s diet.
A small number of children develop red, irritated eyes. Speak to your child’s GP or IBD team if you’re worried about their eyes. You can also go to a high street optician. This could help to avoid a more serious eye problem.
Your child may get a skin rash at the start of a flare-up. For example, they could get small painful red patches on their shins, called erythema nodosum. Skin rashes should go away as your child is treated for Crohn’s or Colitis. But in some cases, treatments for Crohn’s or Colitis can cause skin rashes. Speak to your child’s IBD team if you notice a rash or other skin problems.
Your child might lose more hair than usual for a while. This could be due to a condition called alopecia areata or a condition called telogen effluvium. Both are associated with Crohn’s and Colitis.
If your child is losing more hair than usual, speak to their IBD team to check what might be causing it. Do not stop any medicines before speaking with their IBD team.
Crohn’s and Colitis can sometimes affect the liver, due to a condition called Primary Sclerosing Cholangitis. Some medicines, including azathioprine and methotrexate, can also affect the liver. Your child will have regular blood tests to check for liver problems. A change in medicine type or dose can often help any liver problems that happen.
There were little signs for a while before Crohn’s Disease was diagnosed. Ellie would have a sore mouth, suffered terribly with her skin as well as having bouts of tummy ache, constipation and diarrhoea.
Donna
Parent of Ellie, living with Crohn's
Some children, more commonly children with Crohn’s, may also develop complications. These can include:
These complications can all be treated.
To find out more, see our information on Crohn’s Disease, Ulcerative Colitis, and fistulas.
If Crohn’s or Colitis affects the colon, this can increase the risk of bowel cancer. This sounds scary, but the risk of bowel cancer is still very low in children. This is because the risk only starts to increase around 8-10 years after the start of Crohn’s or Colitis symptoms.
It’s natural to worry about your child’s risk of bowel cancer later in their life. But the actual increase in the risk of developing bowel cancer if they have Crohn’s or Colitis is low. Also, people who might be at higher risk can have regular bowel screening to check for early warning signs. Finding bowel cancer at an early stage gives treatment the best chance of working.
Find out more in our information on bowel cancer risk and speak to your child’s IBD team if you’re worried.
Very rarely, some medicines for Crohn's and Colitis can increase the risk of other cancers. This may sound worrying, and you may wonder if taking one of these medicines is right for your child. It's important to know that the risk of cancer is very small and the benefits of taking these medicines will usually outweigh the possible risk.
There are often ways to reduce the risk of side effects. For example, some medicines can increase the risk of skin cancer. Your child can lower this risk by using high protection sunscreen and protective clothing.
Always read the information leaflet that comes with your child’s medicine. It will have useful information about possible side effects and ways to avoid or reduce them. Speak to your child’s medical team if you are worried.
PSC is an inflammatory condition affecting the bile ducts. Your bile ducts are tubes that connect your gallbladder and liver to your small bowel. Bile ducts carry bile, which helps to digest food. In PSC, bile builds up in your liver, causing liver damage.
Research suggests that almost 1 in 10 people with Crohn’s or Colitis develop PSC, although the real number could be even higher. If your child has PSC as well as Crohn’s or Colitis, you may hear their condition called PSC-associated IBD or PSC-IBD.
PSC is more likely if your child has a lot of inflammation in their large bowel. This means it is more common in people with Ulcerative Colitis or Crohn’s Colitis. PSC is also more common in males than females.
You can get support and information on PSC from the British Liver Trust, PSC Support, or the Children’s Liver Disease Foundation.
Flare-ups can come on suddenly, without an obvious trigger. Your child’s symptoms may be different to previous flare-ups, so keep an eye out for anything unusual. Contact your child’s IBD team if you’re worried they may be having a flare-up. Signs of a flare-up can include:
Your child’s IBD team should work with you to create a flare-up plan. This should include:
They can also tell you about any over-the-counter medicines that could help your child’s symptoms. For example, they may be able to take paracetamol to help with gut or joint pain. But certain other painkillers, such as ibuprofen, could irritate their gut and make some of their symptoms worse. You should only give medicines to your child if your doctor has advised you to.
Some hospitals have an email service or advice line so you can speak directly with an IBD nurse. Others may have a phone number to reach the secretary or leave a message.
You might also be able to use a smartphone app to record your child’s symptoms and send non-urgent questions. Ask your child’s medical team if this is an option.
It’s important that your child has regular check-ups with their IBD team, even if they seem well. Their IBD team will want to test their blood and poo regularly to make sure their condition is under control. How often will vary from child to child, and may change over time, so check with your child’s IBD team if you’re unsure.
The best way to help prevent a flare-up is to encourage your child to follow their treatment plan and take their medicines. See the section on supporting your child for tips on encouraging your child to take their medicines.
For some children, stress can trigger Crohn’s or Colitis symptoms. If your child is going through a stressful time, such as changing schools or taking exams, they may need extra support. See the section on supporting your child for ways to support their emotional wellbeing.
Your child will have already had tests to diagnose Crohn’s or Colitis. They will continue to have regular tests to check their condition. Your child’s IBD team will say how often your child needs tests, and where these will take place. How often will depend on the treatment your child has and how well their condition is being controlled.
Tests may be different in children under the age of 5. This is because Crohn’s and Colitis are uncommon in very young children and less is known about the best ways to monitor and treat this age group. If your child is under 5, speak to your IBD team about the tests that will be used to monitor their condition.
Your child will have regular blood tests to monitor their condition and check it is being controlled. Blood tests can be used to check for:
Our tests and investigations page has information on blood tests.
Your child’s poo will also be tested to monitor their condition and check they’re in remission. It can be checked for signs of bleeding, inflammation and infection in their gut.
Your child’s medical team may check their poo for the amount of a protein called calprotectin. Calprotectin is released into the bowel when there is inflammation. High levels of calprotectin can be a sign that your child’s condition is active and causing inflammation. Calprotectin tests are often used to monitor Crohn’s and Colitis, and to check whether treatments are working.
How often your child has their poo tested will vary, so check with their IBD team if you’re unsure.
Endoscopy is using an endoscope to look inside your child’s body. An endoscope is a long, thin tube with a camera at the end. This test will be done in the children’s gastroenterology unit of a hospital.
The type of endoscopy used will depend on which part of your child’s gut needs to be checked. If the tube goes down their mouth into the stomach, this is a gastroscopy. If the tube goes up their bottom into the bowel, this is a colonoscopy or sigmoidoscopy.
The doctor may also take tiny pieces of the lining of the gut, called biopsies. These biopsies can then be looked at under a microscope. They may also take photos for your child’s medical records.
When Albert had the endoscopy, he was very young, so he couldn't really communicate his feelings. But he handled the test and the hospital visits very well.
Sarah
Parent of Albert, living with Colitis
An endoscopy can feel uncomfortable, but it should not hurt. Children are usually offered a general anaesthetic, so that they’re asleep and cannot feel anything or move around. Older children may be offered a sedative instead, to help them relax.
The hospital should give you details of when and how to prepare your child for their endoscopy. If your child is having a colonoscopy, they may need to eat a low-fibre or liquid diet for a few days before the test. They may also need to take a laxative medicine to clear their bowel. Children often find this uncomfortable, as it can cause tummy cramps. Throughout the preparation, it’s important that your child drinks plenty of water.
Ben had various colonoscopies but they were carried out under general anaesthetic so he knew very little of them, and blood tests have become a routine part of life now.
Bev
Parent of Ben, living with Colitis
Endoscopies can be upsetting for parents, particularly if your child has never had an anaesthetic before. You may find it helpful to find out exactly what will happen before your child’s appointment so that you know what to expect. You can find out more about endoscopies in our information on tests and investigations.
I took so much time preparing Liv for her first cameras that I forgot to prepare myself, and when we took her to theatre for a general anaesthetic I was quite taken aback and upset.
Sarah
Parent of Olivia, living with Crohn’s
Some hospitals may offer a special sort of endoscopy, called capsule endoscopy. Your child will swallow a capsule, about the size of a large jellybean, with a tiny camera inside. This takes photos as it passes through their gut, before leaving the body in their poo.
Your child may have X-rays and other scans to look at their gut. These might include:
For more details, see our information on tests and investigations.
Days spent at the hospital can be stressful. There are some things you can do to make days at the hospital as stress-free as possible:
Treatments for Crohn’s and Colitis aim to make your child feel better, ease symptoms, and keep inflammation under control. There’s no cure or single ‘best’ treatment for Crohn’s or Colitis. Your child may have one or more of the following treatments:
The treatment your child has will probably change over time and will depend on lots of things, including:
This involves drinking a special liquid ‘food’ instead of normal food. You might hear it called:
Examples include Modulen IBD, PaediaSure and Ensure.
If your child has Crohn’s, this will usually be the first treatment they have when they are diagnosed. They might have a liquid diet again if they have a flare-up, or to help them grow.
Some evidence suggests that replacing some food with a liquid diet, while avoiding certain foods, could help mild Crohn’s flare-ups. This treatment is not very common. Your child should only try it if suggested by a dietitian in their IBD team.
If your child has Colitis, a liquid diet will not usually be used to treat their condition. But they may sometimes be prescribed nutritional drinks, to give them extra energy for growth.
If your child has IBDU, a liquid diet might be an option, but this is not very common. Talk to your child’s IBD team about whether it is an option for your child.
Your child will drink a special liquid instead of eating normal food, usually for six to eight weeks. The drinks should be spread out through the day.
We do not yet know exactly how a liquid diet works. But we know it can help with inflammation. This may encourage the gut lining to heal, while giving your child all the nutrients they need to grow properly.
Most children begin to feel better after a few days on a liquid diet. Your child may miss eating solid foods. Try to stay positive and encourage them, as this can be a very effective treatment. Your child’s IBD team can support you and give practical advice on managing your child’s liquid diet.
Your child will slowly start to have normal foods again over a few weeks. Their IBD team, usually a dietitian, will explain how to do this.
My son had two courses of Modulen at the beginning of his treatment. He didn’t like the taste, but it worked well getting him into remission. He now has two Modulen drinks a day, alongside a normal diet, to keep his weight up.
Rachel
Parent of Thomas, living with Crohn's
You can get liquid diets from your local pharmacy with a prescription. Liquid diets come as a ready-made drink or a powder that you mix with water. Most liquid diet products are available in different flavours, or you can add prescription flavourings to plain ones. They may be able to have other drinks too but check with their IBD team first.
Some children get side effects like feeling or being sick, diarrhoea, bloating or wind. If your child feels hungry, contact their IBD team or dietitian.
Some families find having a liquid diet can be hard at mealtimes. Talk to your child before they start, to find out what they want to do. Some children prefer to do something else at mealtimes, rather than sit with the family.
It can also be helpful to discuss what your child wants to do during meals at school. They may be able to take their liquid diet to school, for example in a sports bottle. Check this with their IBD team or dietitian first.
Liv did the eight-week liquid diet on diagnosis. That was quite difficult and I think none of us were quite prepared for what that meant as a family. But we got through it and then it was joyful seeing her eat her first bits of food.
Sarah
Paren of Olivia, living with Crohn's
If your child finds drinking hard, or really does not like the taste, they may be able to have a nasogastric feeding tube. This is a thin tube that goes through the nose into the stomach. Your child’s dietitian or IBD team can help with this. Your child should still be able to go to school or college with a nasogastric tube and take part in their usual activities. Some children feel self-conscious about it, so it could help to speak to their teachers before they get the tube. You can give the feed at a time that suits your child’s daily routine. Some can even be given overnight while your child is sleeping.
Evie has had a liquid diet taken through a nasogastric tube. Although coping with the tube and the diet in everyday life is hard, the results have been really good for her in terms of getting the Crohn's into remission.
Ruth
Parent of Evie, living with Crohn's
There’s more information about a liquid diet in our information on food.
The medicines used to treat Crohn’s and Colitis aim to stop inflammation, treat flare-ups, and stop future flare-ups. Your child’s IBD team will explain which medicine they recommend and why. Older children may find it helpful to talk to their IBD team themselves.
All medicines can have side effects. Your child’s IBD team should explain how the medicine may affect them. Make sure the IBD team know if your child gets any side effects, so they can help manage them.
There are four main types of medicine used to treat Crohn’s and Colitis in children. Your child may take one or a combination of medicines at the same time. The most common medicines used to treat Crohn’s and Colitis in children are listed below. There is also detailed information about each medicine on our webpage about treatments.
|
Type of medicine |
Examples |
Form |
|
5-ASAs, or aminosalicylates These medicines are mainly used for Colitis |
Sulfasalazine, mesalazine |
Tablets, granules, enema or suppository. Enemas and suppositories are medicines given into the bottom |
|
Corticosteroids |
Prednisolone, budesonide |
Tablets, intravenous drip |
|
Immunosuppressants |
Azathioprine, mercaptopurine, methotrexate |
Tablets |
|
Biologics |
Adalimumab, infliximab |
Injection, intravenous drip |
5-ASAs are also known as aminosalicylates. They help with inflammation in the gut so that damaged tissue can heal.
If your child has Colitis, they will probably have 5-ASAs when they are first diagnosed. They may take them every day for several years, even when they are well.
If your child only has inflammation in the lower part of their colon or rectum, they may have an enema or suppository. An enema is a liquid medicine that goes into their bottom, while a suppository is a tablet that goes into their bottom.
Your child may not want to try an enema or suppository at first. But they work well and get the medicine straight to where it is needed to help them feel better.
Enemas and suppositories can be difficult to use at first. Get support from your child’s IBD nurse when trying this type of medicine for the first time.
5-ASAs are sometimes given to children with Crohn’s, but this is less common. They might be an option if your child has been diagnosed with IBDU.
Read more about 5-ASAs.
Our daughter has been treated with mesalazine for a while. It has worked well for her and she hasn’t experienced any side effects.
Andrew
Parent of Emma, living with IBD Unclassified
Steroids can help to control inflammation. They can be given as a tablet, liquid, or a drip into the arm. They are not the same as anabolic steroids used by athletes to improve their performance.
Your child might have steroids:
If your child has Colitis, they’ll usually only have steroids if 5-ASAs are not right for them or have not helped.
Steroids are very effective and can act quickly to make your child feel better. But they can cause side effects, so doctors will try to give the lowest dose that works, and for as short a time as possible. It’s important to follow the instructions given by your child’s IBD team. Your child should not stop taking steroids without talking to their IBD team.
Steroids can also affect a child’s growth and can make teenage acne worse. Some children may become irritable, moody, or have temper tantrums. You can find out more in our information on steroids.
Anyone who treats your child for another illness or injury needs to know they take steroids. Your child should carry a ‘Steroid Treatment Card’. You can get one from your GP practice, hospital or pharmacy. Or your child could wear an emergency bracelet, available from pharmacies or online.
These include azathioprine, mercaptopurine and, less commonly, methotrexate. These medicines help with inflammation in the gut by dampening the immune system, so that it does not attack the body’s own tissues. They can take two to three months to start working, so they are not used on their own as a first treatment or to treat flare-ups. But they can help to reduce the risk of flare-ups and keep your child in remission.
If your child has Colitis, they may have immunosuppressants alongside a 5-ASA medicine. Or they may have an immunosuppressant if 5-ASAs are not helping.
We have more information on azathioprine, mercaptopurine and methotrexate that you may find useful.
On the whole, my son’s experiences of drug treatments have been quite positive. He did have some side effects with azathioprine, such as being very tired and getting aching joints, but we’ve minimised these by taking it at bedtime.
Bev
Parent of Ben, living with Colitis
Biologics act on the immune system, but in a different way to immunosuppressants. They work by blocking certain proteins or processes that are involved in inflammation. Your child may have a biologic medicine if other medicines have not helped.
The two most common biologics are:
Your child will need tests before taking a biologic medicine, to make sure they do not have any hidden infections.
You can find out more about the biologic your child may be offered in our treatment information.
It can take a long time to find the right medicine, or combination of medicines, that work for your child. Your child may try one or more treatments that do not help, before finding one that does. This can be frustrating but is quite common. Ask your child’s IBD team how long it should take for their treatment to work and contact them if it does not help.
Immunosuppressants and biologics can make your child more sensitive to sunlight. Make sure your child is properly protected by covering them up, keeping them in the shade and using a high protection sunscreen.
The thought of your child having surgery can be worrying. But surgery is an important treatment option that can help your child feel well again. Some research suggests that around 2 in 10 children with Crohn’s, and nearly 1 in 10 children with Colitis may need surgery.
Surgery may be an option if your child:
If you are thinking about surgery, the IBD team will refer your child to a surgeon. The surgeon will explain the operation and talk through any concerns. Your child may be able to have keyhole surgery known as a laparoscopy, where only small cuts are made. People usually recover faster and have less pain after keyhole surgery, but it is not always an option.
Surgery should only happen after careful discussion between you, your child and their IBD team. You can read more in our information on surgery for Crohn’s Disease and surgery for Ulcerative Colitis.
George has coped really well with his Crohn’s diagnosis. It has been hard, but we have adapted as a family, and given him our full support. Including, as he’s getting older, encouraging him to take his medication himself.
Warren
Parent of George, living with Crohn’s
It’s important to take care of your child’s emotional and mental health as well as their physical health. Feelings of anxiety, low mood and stress can affect many parts of their everyday life. This could include their school, social and family life, confidence, self-esteem and sleep. Poor mental wellbeing could stop them taking medicines properly and make symptoms like pain and fatigue worse.
There are some things you can try to help your child cope with their condition.
Having Crohn’s or Colitis will mean some changes in your child’s life. But wherever you can, try to live as normal a life as possible. Routines are important for children. Try to keep doing your usual family activities but be prepared to change your plans at the last minute if your child is too tired or unwell. If your child is disappointed, you can reassure them that you’ll do those activities or outings when they feel better.
We’ve put a lot of focus on making home a calm, stress free and fun space. Whether it be a good day or a difficult IBD day, we all feel comfortable and relaxed. I think this has contributed to reducing the severity of symptoms and has meant that we all respond to changes in a calm way.
Rob
Parent of Harry, living with Crohn’s
Your child, like you, will probably need time to get used to their diagnosis. Explain what’s happening in words your child understands. Be as honest as possible. If something’s going to hurt, say so. But also explain that it’ll help them feel better in the long run. For example, you might tell them: ‘The needle will feel like a sharp scratch, but it’ll be over before we can count from ten to one. Then the doctors and nurses will be able to help you.’
Harry knows all of the possibilities and consequences, like one day he might need surgery. Even though he’s only 11, this openness has made him quite pragmatic and he doesn’t fear that possibility.
Rob
Parent of Harry, living with Crohn's
Some parents have difficulty in getting healthcare professionals to take their child’s symptoms seriously. In these situations, it’s important to listen to what your child is saying and keep pushing for answers. You might want to read about Stacey’s experience of getting her son, Louis, his diagnosis.
If I was asked what advice I’d give to other people trying to advocate for their loved ones who are experiencing symptoms – just keep pushing. Keep pushing for answers and don’t be afraid to be ‘a pain’.
Stacey
Parent of Louis, living with Crohn’s
It may helpYour child might enjoy reading, audiobooks, computer games, films, or learning a new craft or instrument. If they’re old enough, you can find free lessons for most things on YouTube.
Encourage them to make the most of the times when they’re feeling healthy. You could tell them about people whose Crohn’s or Colitis has not stopped them from having exciting lives. Examples include magician Dynamo, racing driver Jonny Edgar, Strictly dancer Amy Dowden, and former footballer Darren Fletcher.
I was diagnosed with Crohn's Disease when I was 19 years old, although I started suffering with the symptoms from the age of 12. I have always been driven to win, so Crohn’s wasn’t going to hold me back.
Amy Dowden
Professional on Strictly Come Dancing, living with Crohn's
Children may feel less isolated if they can talk to others in a similar situation. You may be able to meet other families through the Crohn’s & Colitis UK Local Networks and events across the UK. The charity CICRA has an E-Pal scheme, which gives children a chance to chat with other children with Crohn’s or Colitis.
There are lots of things about Crohn’s or Colitis that your child cannot control. But you can give them choices about their care, when possible. This can help them feel more in control. For example, which arm they’d prefer the needle in, or what they’d like to do after taking their medicine.
Show them simple ways to manage their condition. Younger children could put on their own ‘magic cream’ to numb their skin before blood tests, or their own plaster afterwards. Older children could gradually have more responsibility for managing their own medicines.
Try taking a doll or teddy along for blood tests. It could help to pretend that the toy is a patient and use it to explain what will happen.
Children’s nurses at the hospital are often used to encouraging this type of play. But appointments at the GP surgery are often shorter, and the practice nurses may have less time to prepare your child or use toys. In this case, it may help to arrive early so that you have extra time to play and prepare your child while you wait.
At times, having a sense of humour could help your child feel better. It might help them realise that their symptoms are not embarrassing. Some parents tell us that it’s good to laugh about things, as long as the child feels comfortable and does not think you are laughing at them.
If you’re worried that your child is not coping with their diagnosis, it may help them to talk to a psychologist or counsellor. Their IBD team might be able to help with this.
Your child will experience ups and downs, just like any other child. But you might notice more worrying changes in their mood or behaviour at times. Signs they may be struggling include:
Encouraging your child to talk is an important first step. They may find this difficult, so keep trying and stay positive and encouraging. Make sure they know that you want to listen and choose a time when there are few distractions. Younger children may find it easier to draw what’s worrying them. Teenagers may be more likely to open up if you’re side by side, for example sitting in the car or going for a walk.
Your child may find it easier to talk to another trusted adult, such as a close family member, someone in their IBD team, or their favourite teacher. Whoever your child chooses to talk to, discussing their worries can help them to see things differently and find ways to cope.
Parents and healthcare professionals have found several ways to support children’s emotional wellbeing. There may be something here that could help your child:
If you’re concerned about your child’s emotional wellbeing, talking to a counsellor might help them. Check if your child’s IBD team has a counsellor or clinical psychologist or ask if they can refer your child to one. Your GP practice or child’s school may also have a counsellor. Your child could also speak to someone on a helpline such as Childline, or Children First in Scotland.
Young Minds has a helpline for parents and adults worried about a child’s mental health. And our information on mental health and wellbeing has more about what counselling is and how it can help.
It’s important for your child to take their medicines as prescribed, to keep them well and prevent flare-ups. This can be difficult for children. Some parents have told us their children rebel, while other children may simply forget. Children who do not take their medicine are at a higher risk of flare-ups and severe disease. Parents can play an important part in helping their child take their medicines. Some of the following ideas may help:
Try to remind your child why it is important for them to take their medicine.
There are lots of resources and services that may be helpful for children living with Crohn’s or Colitis.
Meet our Crohn’s and Colitis cats
A colourful story book and animation to help explain Crohn’s and Colitis to children. You can watch the animation or download the book on our website.
This has basic information about Crohn's or Colitis for anyone who is new to the condition. The easy-to-read format makes this a useful resource for teenagers and young people.
‘What are Crohn’s and Colitis?’ animation
A two minute animation explaining the basics of Crohn’s and Colitis.
Your child can create their own Talking Toolkit to help them find the words to talk about Crohn’s or Colitis to their teachers and friends.
‘Telling my friends’ animation
An animation based on research with young people with Crohn’s or Colitis, funded by Crohn’s & Colitis UK.
Five young people discuss challenges such as school, university and relationships, and share their own ways of coping.
Transition: moving to adult care
A guide for older children moving to adult care, written with the help of other young people.
16 to 18 year olds are eligible for concessionary Crohn’s & Colitis UK membership. This means membership is cheaper or free, depending on your situation.
CICRA are a charity that support children with Crohn’s or Colitis to live as normal a life as possible. Their website has information and videos for children and young people.
Over The Wall offer free weekend activity camps for children and young people with health conditions and their families. They even offer camps for siblings.
Crohn’s and Colitis are often described as invisible conditions. Your child might look fine on the outside, even if they have painful or distressing symptoms. This can make it hard for other people to know how unwell they are, but it’s up to you and your child how much you tell family and friends.
Negative reactions may be more likely when a person does not understand the condition. Other parents may be unsure of what your child can eat. Some might even worry that the condition could be infectious.
I did initially get a bit cross having to explain everything to people who seemingly couldn’t understand. But I didn’t know anything about IBD until it impacted my family, so you need to bear that in mind when speaking to others and be patient.
Stuart
Parent of Charlie, living with Crohn's
Being open and honest is usually the best way to tackle any confusion. It could help to talk to your child’s friends, or their parents if the friends are young. Check that your child is happy with this first. You’ll probably find that most people are supportive once they know how they can help.
We know it can be difficult to talk about Crohn’s and Colitis. We’ve put together lots of tips to help start conversations in our Talking Toolkit.
Being able to get to a toilet can be a worry for people with Crohn’s or Colitis. Here are some ways to help your child feel more confident when out and about:
Eating with Crohn’s or Colitis is different for everyone. Apart from a liquid diet for Crohn’s, no single diet has been proven to help in the long term. The main thing is for your child to eat a healthy, balanced diet when they can. This is essential for their continued growth and development. A Mediterranean diet is one example of a healthy diet that includes all the nutrients your child needs. They should also drink plenty of water to avoid getting dehydrated.
Some children find that certain foods trigger their symptoms or make them feel worse when they’re in a flare-up. Common examples include spices, herbs, dairy products, and high-fibre foods such as vegetables, nuts and wholegrains. But everyone is different.
If you think a particular food is affecting your child, try keeping a to record what they eat and any symptoms they get afterwards. It may help your child to avoid certain foods that upset their gut. If Crohn’s is affecting your child’s mouth, it might help to avoid cinnamon and benzoates. Cinnamon and benzoates are found in some processed foods and fizzy drinks. But you should always talk to their doctor or a dietitian before cutting out any foods, to make sure your child does not miss out on important nutrients.
Regular blood tests will show if your child is low in any vitamins or minerals. If needed, their doctor will prescribe supplements or nutritional drinks. Your child should not need to take extra vitamins or minerals, unless advised by their doctor.
Our information on food has more details on healthy eating with Crohn’s or Colitis. Your child’s IBD team may also be able refer you to a dietitian.
Children with Crohn’s or Colitis may be thin or underweight. Your child may lose interest in food if they’re having a flare-up. They may be scared to eat if this might cause symptoms or make their symptoms worse.
It can be difficult for a child with Crohn’s or Colitis to eat enough to reach their ideal weight and height. Your child’s IBD team may recommend nutritional drinks to top up their calories. Speak to your child’s IBD team if you are worried.
Some people with Crohn’s or Colitis may start to refuse certain foods, without advice from a dietitian. Sometimes, this behaviour can become extreme and lead to an eating disorder called ARFID.
ARFID is when someone avoids certain foods, or limits how much they eat. We do not yet know how common ARFID is, but some research suggests it may affect almost 2 in every 10 people with Crohn’s or Colitis. It could increase your child’s chances of malnutrition, where the body does not have enough of all the nutrients it needs.
Your child might develop ARFID if they think certain foods have made their Crohn’s or Colitis symptoms worse. Or if they get anxious or afraid when they eat.
Tell your child’s IBD team if you notice them avoiding or refusing any foods. They may suggest a referral to a dietitian, or to Child and Adolescent Mental Health Services (CAMHS), for specialist support.
The charity Beat has more information about ARFID.
Patrick’s diet is restricted due to sensory difficulties. He has ARFID, he has an aversion to anything he doesn’t know. All he eats is bland food. The guilt of me feeding him pizza and sausages when I know this is not healthy, but it’s all he will eat, it’s not easy.
Andreea
Parent of Patrick, living with Colitis, autism and ARFID
Sports and exercise are a big part of life for many children, and your child should still be encouraged when they are well. Exercise can have positive effects on mood, self-esteem, sleep quality and energy. In a study of Crohn’s & Colitis UK members, 7 in 10 said that exercising made them feel better. Early research also suggests it may help to improve bone health in children with Crohn’s or Colitis. You can find out more about exercising with Crohn’s or Colitis in our information on being active.
If you’re not sure whether your child should take part in certain activities or sports, speak to their IBD team.
Fatigue is an overwhelming feeling of tiredness, low energy and exhaustion that does not go away after rest or sleep. It’s very common in people with Crohn’s or Colitis. Fatigue can have a big impact on your child’s school, social and family life. Your child may need to take more time out, pick and choose what they do, and learn that it’s OK to say no to things.
Fatigue can be difficult to manage. Some people say they find some of the following things helpful:
It can be hard to know exactly what is causing fatigue. For example, it could be caused by inflammation, some medicines, or low levels of certain nutrients. If your child is struggling, speak to their IBD team. They may be able to suggest ways to help your child manage their fatigue or prescribe supplements if needed.
See our information and animation on fatigue for more information and support.
Weekends are planned so that Evie doesn’t get too tired. We make sure that she has some time to rest in between doing things.
Ruth
Parent of Evie, living with Crohn’s
School is a key part of your child’s life and it’s important for them to go as much as they can. Some children do not want to tell people about their condition. But telling your child’s school can help them understand your child’s condition and needs.
Get in touch with the school and ask to create a plan together, to help manage your child’s condition at school. You might want to ask for a meeting with you, someone from the school, and a member of your child’s IBD team. This can be a quick and simple way to make sure everyone has the same information.
Try to build a good relationship with your child’s form teacher and the person who arranges learning support. This person is likely to be:
This can make it much easier to raise problems and find solutions if needed.
Ask them to read the information on our website, including the information on supporting students. You may find it helpful to give copies of their resources for schools to your child’s school, so that staff know how to support your child.
Make sure staff have any information they need about your child’s treatment. This includes possible side effects and ways to manage them. Tell them if your child’s medicine affects their immune system, so they can let you know about any illnesses in your child’s class.
Some schools have strict rules about using the toilet during lessons. Your child might need a ‘toilet pass’ so they can leave class whenever they need the toilet. Contact your child’s school to arrange this as soon as possible. They may ask for a signed letter from a healthcare professional. Your child’s GP or IBD team can help with this.
The head of year has been helpful. He gave Charlie a card which means he can use the toilet any time he needs to. He also has access to staff facilities that are more private.
Donna
Parent of Charlie, living with Crohn’s
Make sure your child’s teachers know that your child may sometimes need the toilet suddenly. They may have to leave the class more than once, or for a long time. They might also miss the start of lessons if they’re in the toilet. Knowing this means your child’s teachers will not tell your child off or ask questions that could be embarrassing.
Feeling unwell or tired could make it harder for your child to do their homework and hand in projects on time.
The school also need to understand that Crohn’s and Colitis are unpredictable. Your child will hopefully be well for long periods of time. But they may also have times when they are unwell. They might have to go home early or not go into school, sometimes for days or weeks at a time.
Speak to your child’s teachers about their schoolwork. If your child feels well enough, the school may be able to send work by email so that they do not fall behind.
Schools have a legal responsibility towards children with medical needs. Relevant laws include the Equality Act 2010 in England, Wales and Scotland, and the Disability Discrimination Act 1995 in Northern Ireland. Crohn’s and Colitis are not disabilities. But if your child has severe Crohn’s or Colitis, the law may apply to them. Schools in England must also support children with health problems under the Children and Families Act 2014.
The following organisations have more information to help you get your child the education they are entitled to:
I've got the school where I need them to be now. I typically email the form tutor and the Special Educational Needs Coordinator (SENCO) every term, reminding the school of reasonable adjustments that need to be made. I had to go super formal with them really.
Stuart
Parent of Charlie, living with Crohn’s
For many children, schools can arrange enough support to meet their needs. But some children need more complex support.
England
If the school cannot meet your child’s needs, you can ask your local authority to assess your child for an education, health and care plan, known as an EHC plan. This is a legal document that describes your child’s educational, health and social support needs. You can read more on the GOV.UK website.
Wales
You can ask your child’s school to prepare an individual development plan (IDP) for your child. This is a legal document that describes your child’s learning needs, the support your child should get, and who will provide it. If the school cannot provide this support, it can ask the local authority to take over your child’s IDP. Read more on the Welsh government website.
Northern Ireland
Your child’s school may prepare an individual education plan, known as an IEP, or personal learning plan (PLP) for your child. If this does not meet your child’s needs, you can ask the Education Authority to assess your child. The Education Authority may then give your child a Statement of Special Educational Needs. This is a legal document that describes your child’s needs and the support that the Education Authority must arrange. Read more at NI Direct.
Scotland
You can write to the person who arranges extra support at your child’s school, asking them to assess your child’s needs. They may work with you and your child to create a written plan. If the school does not agree, or your child does not get enough support, contact the local authority. You can ask them to assess your child for a legally binding coordinated support plan, also known as a CSP. Read more at Education Scotland.
Children all feel differently about how much they want their friends or other children at school to know about their condition. Some find it helpful if a teacher explains their condition to the class. Others may find this upsetting. Talk to your child about this and ask what they want to happen.
It’s important to help prepare your child to talk about their condition and answer friends’ questions in their own words. You might want to practice these conversations at home, so that your child gets used to talking about their Crohn’s or Colitis.
We talked a lot in advance of school return to help prepare my son. Most questions at his school have been about absence. ‘Why are you studying at home, why can’t you do PE’, rather than toilet frequency.
Stuart
Parent of Charlie, living with Crohn's
If your child is young, they could share our Meet our Crohn’s and Colitis cats story book or animation with their class.
Stress can make some children’s symptoms worse. Try to offer your child extra support during exam periods. Encourage them to find a balance between doing enough studying and staying well. Having regular breaks in revision is important. Some of the suggestions in the section on your child’s emotional wellbeing may also help them cope with stress during exam time.
Let your child’s school know that their condition is unpredictable and can make exams and deadlines harder. Ask to speak with the school’s exams officer so that you can explain your child’s condition and the support they may need. Some schools or colleges may be able to make special arrangements, like delaying internal exams or dates for handing in work. Some children may be able to do exams in a separate room near to a toilet. Or they might be given extra time to make up for toilet breaks.
I booked a face-to-face appointment with the exams officer at the school as GCSE mock exams were being scheduled, to ensure relevant adjustments were made. These included a seat near the exit, time out to go to the bathroom, and time added on at the end.
Stuart
Parent of Charlie, living with Cohn's
Children can sometimes say or do things to hurt another child, often targeting them for being ‘different’ in some way. Children with an illness are more likely to be bullied. It can help to be aware of the possible signs of bullying. Many are the same as those for depression, anxiety or stress. Other possible signs include:
There can be lots of other reasons for the things mentioned above. If you’re worried, encourage your child to talk to you, or another trusted adult.
If they are being bullied, try to stay calm and reassuring for your child. Be clear that bullying is not OK and reassure them that you can help. Get in touch with their teacher and make sure your child knows what to do if it happens again.
The charities Family Lives and Young Minds have more information on what to do if your child is being bullied. They also have helpline services for parents.
Your child should still be able to go on holidays or visit family overseas. It may just take some extra thought and planning.
We have travelled with our son, but we prepare well in advance. We always take a letter from his consultant with us, outlining his condition and medication, just in case.
Rachel
Parent of Thomas, living with Crohn’s
Our information on travelling cover things to think about before travelling. It includes information on travelling with a stoma and tips for staying well on holiday.
It’s important that your child has routine vaccinations. These include:
These vaccines are usually safe for children with Crohn’s or Colitis but always check with your child’s IBD team first.
All children with Crohn’s or Colitis should have a flu vaccine every year. Most children are offered the children’s nasal spray flu vaccine at school until they are 15. If your child is on certain steroids, immunosuppressants or biologics, they cannot have the nasal spray vaccine. This is because it is a live vaccine. Your child should have a flu vaccine injection instead, as this is not a live vaccine.
Your child probably cannot have live vaccines if they take steroids, immunosuppressants or biologic medicines that weaken the immune system. Live vaccines include:
Speak to your child’s IBD team about these.
If your child stops taking a medicine that weakens their immune system, they may have to wait three to six months before they can have a live vaccine. If someone living with your child is due to have a live vaccine, ask their IBD team if they need to take any special precautions.
COVID-19 vaccines are safe for people with Crohn’s or Colitis. Your child may have a reduced response to the vaccine or lose protection faster if they’re taking medicines that weaken the immune system.
Find more information about COVID-19 for people with Crohn’s or Colitis.
Some travel vaccines, including yellow fever, are live vaccines. Your child may not be able to have live vaccines if they’re taking a medicine that weakens their immune system. Speak to your child’s GP or a private travel clinic at least eight weeks before you travel. You can also ask your child’s GP for more general advice about travel health, such as protection against malaria.
Supporting a child with Crohn’s or Colitis can be more challenging if they are autistic or have attention deficit hyperactivity disorder (ADHD). Each child may be affected in different ways.
My son is autistic, so this complicates things. He needs us more in terms of care and wiping his bum. Implementing a healthy diet or accepting a new medication, or anything new for that matter, is a challenge.
Andreaa
Parent of Patrick, living with Colitis and autism
Talk to your child’s professional teams
Speak to both the IBD team and the specialists who help with your child’s autism or ADHD. They can help identify issues that might affect your child’s care, and work with you and your child to overcome them.
For example, your child might be able to see the treatment room and equipment before their appointment, so they know what to expect. Or, if your child struggles in noisy waiting rooms, staff may show you to an empty side room or the hospital’s prayer room instead.
Encourage coping strategies
Remind your child to try their usual ways of coping with the world around them. Make sure they take any helpful items they need to appointments, such as headphones, fidget toys, or an eye mask.
Get a sunflower lanyard
A sunflower lanyard shows people that your child has an invisible condition and may need extra support or understanding. You can get a sunflower lanyard and find out more about the scheme from Hidden disabilities.
Learn to spot signs of discomfort
It can be difficult to know when your child is in pain or unwell if they do not use words. It may help to look for physical signs, such as bloating, wind, diarrhoea, constipation or smelly poo.
Your child’s behaviour may change when they have symptoms. They may get more irritable or anxious, react more to noises or bright lights, or have trouble sleeping. Non-verbal children may scream, sigh, whine or moan. Younger children may become aggressive. Learning to spot these behaviours could help you to understand your child’s symptoms.
Ask to see a psychologist
Autistic children often struggle to communicate and deal with their emotions. A psychologist could help them to open up and feel more positive. Psychological support could also help if your child has sensory issues that affect their eating or use of medicines. Your child’s IBD team may be able to help with access to a psychologist.
The following organisations and websites may have useful information or services to help you support your child:
Autism Central: www.autismcentral.org.uk
National Autistic Society: www.autism.org.uk
As your child gets older, it’s important that they start to take control of managing their condition. Your child’s IBD team will encourage them to take more responsibility as they reach their teenage years. This is part of the ‘transition’ process: preparing to move your child’s care from child to adult services. The formal transfer usually happens when a child is around 16, but can happen a little later. For example, your child’s IBD team may decide to wait if your child is currently having a bad flare-up or is doing exams.
I think it is vital that Ellie is involved in the everyday management of her Crohn’s, which will continue through her adult life. Encouraging her to ask questions helps her feel she has more control over her condition.
Donna
Parent of Ellie, living with Crohn's
Each hospital manages transition differently. Some have special clinics for 16 to 19 year olds, some offer one or two joint appointments with staff from both services, and some just send a letter. Your child should have their own transition plan, made together with their IBD team. Ask about the process at your child’s hospital.
There are lots of ways you can help your child prepare for transition. Start by letting them take more control of their medicines over time. You could sit down together before appointments and encourage them to think of their own questions to ask their IBD team. You could even let them meet their IBD team alone every now and then. This will help them to be more confident and independent by the time they meet their new IBD team in the adult clinic.
Your child might find it helpful to read our information for teenagers on transition: moving to adult care. Our appointment guide can also support them in taking control of their own appointments.
Your child’s IBD team understand that their diagnosis may be challenging and distressing for the whole family. Looking after a child with Crohn’s or Colitis can feel overwhelming at times. It can affect all parts of your life, from family life and relationships to work, finances and leisure time. It can also have a major impact on your emotional wellbeing. For example, some parents say they feel isolated and alone when their child is first diagnosed, or during long periods of illness. Some parents we’ve spoken to describe a feeling of grief for the future they had expected for their child, or guilt that they cannot make their child better. The ‘up and down’ nature of Crohn’s and Colitis can leave them feeling anxious and on edge.
IBD teams can include different types of professionals, depending on the hospital. Your child’s team may include:
Try to build a good relationship with your child’s IBD team as early as possible. You’ll probably see them regularly for some years and they are an excellent source of information and advice. Your child will also need to develop their own relationships with their team over time.
You will not always have as much time as you would like to talk to your child’s IBD team. Write down any questions you have in advance, so you do not forget them. It’s useful to put these in a list, so you can ask them quickly and easily. Our appointment guide has other useful tips to help you get the most out of appointments.
If you are concerned about your child’s care, you may wish to contact the following for further support:
If you have serious concerns about your child’s diagnosis or treatment, you can ask the IBD team or GP to refer you to another specialist. Seeing another specialist can take a long time. It will depend on how long the waiting list for the hospital is.
You may find it helpful to look at the IBD Standards. These set out what high-quality care looks like at every point from getting diagnosed, through to treatment and ongoing care.
It is not always easy to ask for help. Your family and friends may want to help but just do not know how. You could encourage them to visit our website to read all about Crohn’s or Colitis.
Think about how your family and friends can best support you. You could ask them to:
Many parents say that while family and friends try to understand, it’s impossible unless your own child has Crohn’s or Colitis.
The charity CICRA hold family information days several times a year. These are a chance for parents and young people to meet and share experiences with others in a similar situation. Visit CICRA to find out more. Some hospitals also hold events so that people can meet other local families.
Some parents tell us they find it helpful to chat in and get support from online forums made for parents of children with IBD. But it’s important to remember forums are often not moderated and should never be used for medical advice.
I chat with friends, but unless somebody is actually going through it, I don’t think they can fully understand how stressful and worrying it can be. A great support network I came across, via a magazine, is a Facebook group. These are the people that actually know what you as a parent are going through and there is so much advice, it really helps to interact with people going through similar experiences.
Kelly
Parent of Luca, living with IBD Unclassified
People have different ways of coping with the impact of Crohn’s and Colitis. It may take some time to find what works for you.
If you need support for yourself, you may want to speak to someone who is professionally trained, such as a counsellor or a psychologist. Your child’s IBD team may include a psychologist. If so, they may be able to support you. Your GP can also refer you to local counselling services, also known as talking therapies.
In some parts of the UK, you may be able to refer yourself for free talking therapies.
You can also pay for private counselling. The British Association for Counselling and Psychotherapy can help you find a counsellor in your area.
NHS Every Mind Matters also has tips for looking after your mental health.
You may find that you’re spending more on utility bills, laundry, special diets, travelling to appointments, and lost days at work. Disability Living Allowance (DLA) can help to cover these extra costs. DLA is available for children under 16 who need more care or help than other children. See our information on claiming Disability Living Allowance to check if your child could be eligible, and for information on how to apply.
If you live in England you may also be eligible for the WaterSure scheme. The WaterSure scheme is for people on benefits who need to use lots of water for medical reasons. See Citizens Advice for more information on who is eligible and how to apply.
Students at university may be able to apply for Disabled Students’ Allowance (DSA). DSA can help meet the extra expenses that come with their condition, such as the cost of an ensuite room.
Disabled Students’ Allowance has meant that our daughter has been able to live in ensuite accommodation at university, rather than halls of residence with shared bathroom facilities. It has made a big difference.
Andrew
Parent of Emma, living with IBD Unclassified
Our information on finances explains other financial help that could be available.
It’s up to you how much you tell your employer about your child’s condition. Check if your workplace has any policies in place for taking time off to care for your child. They may offer more time off than the legal minimum, or let you work flexible hours.
If you are worried that your employer might not understand, ask them to read our information. This may help them to understand your child’s condition and the impact on your daily life better.
All employees have the right to unpaid time off work to deal with unexpected events involving their child. For example, if a child is suddenly unwell and needs a day off school. This includes permanent, temporary, full-time and part-time employees. There’s no limit on how many times you can take unplanned time off, but it must be reasonable.
GOV.UK has more information on taking time off work if your child needs you unexpectedly.
There is no legal right to time off if you knew about a situation in advance, such as taking your child to a planned hospital appointment. Some employers may let you make up the hours at another time, or you may get unpaid parental leave. If not, you will need to take annual leave.
You may be able to take unpaid parental leave to look after your child, for example to be with them in hospital. You may be eligible if you are an employee, have been at the company for at least a year, and have parental responsibility. There are limits on how much parental leave you can take and how much notice you must give your employer. Read more at GOV.UK and check your workplace policy on parental leave.
You and your employer may consider other options, such as having flexible start and finish times or working from home.
If you’re unsure of your rights, the charities Citizens Advice and Working Families offer free advice.
We follow strict processes to make sure our information is based on up-to-date evidence and is easy to understand. We produce it with patients, medical advisers and other professionals. It is not intended to replace advice from your own healthcare professional.
We hope that you’ve found this information helpful. Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishop Square, Hatfield, AL10 9NE. Or you can contact us through our Helpline by calling 0300 222 5700
We do not endorse any products mentioned in our information.
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
