When treating Crohn’s or Colitis, the first aim of treatment is to get your symptoms under control. This is induction treatment. Once your symptoms are under control, the aim of treatment is to keep them under control. This is maintenance treatment.
Some clinical trials look at how well a medicine works as induction treatment. Some look at how well it works as maintenance treatment. Some look at how well it works for both.
Find out more about how we talk about the effectiveness of medicines.
Methotrexate in Crohn’s
For Crohn’s, we have information about how well methotrexate works for induction treatment and maintenance treatment separately.
Getting Crohn’s under control
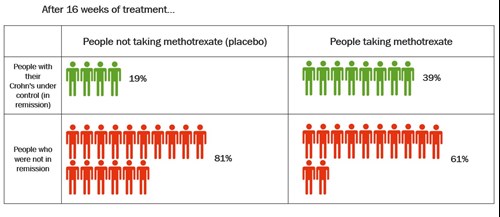
These results come from a review that combines the results of several studies. The review compared methotrexate injection 25mg each week with dummy treatment (placebo). The table below shows how well methotrexate got Crohn’s under control after 16 weeks.
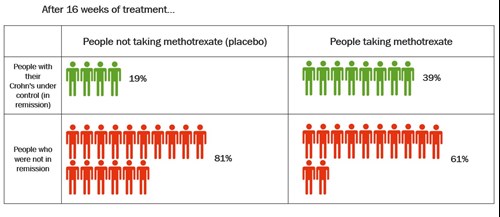
Click to view at full size
After 16 weeks, twice as many people taking methotrexate had their Crohn’s under control compared with those who took placebo. About 39% (39 in every 100 people) who took methotrexate had their Crohn’s under control compared with 19% (19 in every 100 people) who took placebo.
People who took methotrexate needed less steroids to control their symptoms than those who took placebo. After 16 weeks, the people that took methotrexate needed 50% less steroid dose than those who took placebo.
Methotrexate can be as effective as azathioprine, another treatment for Crohn’s. One study compared methotrexate with azathioprine for getting Crohn’s under control. It found a similar amount of people in each group had their symptoms under control after 3 months and 6 months. People taking azathioprine had fewer side effects than those taking methotrexate.
Keeping Crohn’s under control
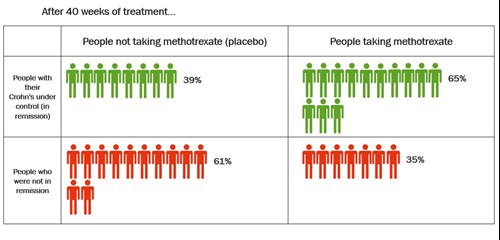
One study compared methotrexate 15mg each week with dummy treatment (placebo) for keeping symptoms under control. The people in the study were already in remission after initial treatment with methotrexate. The table below shows how well methotrexate kept their Crohn’s under control after 40 weeks.
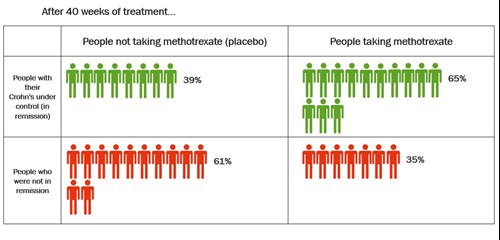
Click to view at full size
After 40 weeks, more people taking methotrexate had their Crohn’s under control than those who took placebo. About 65% (65 in every 100 people) who took methotrexate had their Crohn’s under control. About 39% (39 in every 100 people) who took placebo had their Crohn’s under control.
Fewer people taking methotrexate needed to take a course of steroids for a flare-up.
Methotrexate in Ulcerative Colitis
In people with Colitis, studies show that methotrexate is similar to placebo for induction and maintenance of remission.