Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last full review: March 2023
Next review date: March 2026
This information is for people with Crohn’s or Colitis who are taking steroids. It is also for anyone who is thinking about starting treatment with steroids. Our information can help you to better understand and manage treatment with steroids. It looks at:
This information might use words you have not heard before. Our page on medical words can help provide an explanation.
This information is about steroids in general. It should not replace advice from your IBD team.

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Steroids are also known as corticosteroids. There are many different types, which you take in different ways. The type of steroid you have will depend on how severe your Crohn’s or Colitis is, and which part of your gut is affected.
Oral steroids are medicines you take by mouth. They include:
Intravenous (IV) steroids are given into a vein. You have these in hospital. They include:
Rectal steroids are medicines you apply to inflamed areas inside your bottom. They include:
Steroids are hormones produced naturally in your body. The steroids used to treat Crohn’s and Colitis, are man-made versions of these hormones. The doses you take are much higher than your body makes. At these higher doses, steroids decrease activity of your immune system. This reduces inflammation.
The steroids used to treat Crohn’s and Colitis are not the same as the anabolic steroids used by athletes to improve their performance.
Prednisolone and methylprednisolone are standard oral steroids. They enter your bloodstream soon after you take them. This makes them useful for treating severe or more widespread flare-ups. But it also means they can affect your whole body and cause a range of side effects.
Beclometasone dipropionate (Clipper), budesonide (Budenofalk) and budesonide-MMX (Cortiment) work a bit differently. They are oral medicines, but the steroid in them is not released until it reaches your bowel. This means they work directly on the affected area of your bowel. Very little gets into your bloodstream. So the risk of side effects is lower than with standard oral steroids. You may see them called delayed-release or prolonged-release tablets.
Rectal steroids, which you apply to your bottom, are also designed to work on the affected area. This means they also have fewer side effects than standard oral steroids.
Intravenous steroids go straight into your bloodstream, so work much faster. You will only have these if you need urgent treatment.
If you have a flare-up of Crohn’s or Colitis, steroids can help to quickly reduce the inflammation in your gut. This can help you to feel better and get your symptoms under control. This is known as induction of remission.
Steroids should not be used to keep you in remission. Once your symptoms are under control your doctor will aim to switch you to a different medicine.
Steroids cannot be used long term but can be very helpful during flare-ups. So don’t be afraid to try them if your doctor recommends and keep them updated on your symptoms.
Divya
Living with Ulcerative Colitis
You may have steroids when you’re first diagnosed with Crohn’s, or if you’re having a flare-up. You may be prescribed oral budesonide if you have a mild to moderate flare-up affecting the end of your small bowel. If you have a flare-up affecting your large bowel, you may need standard oral steroids.
You may have steroids if you’re having a flare-up of Ulcerative Colitis. Your doctor will usually only offer you steroids if aminosalicylates (5-ASAs) are not right for you. Or if they have not controlled your symptoms on their own. The type of steroid you take will depend on the part of your bowel affected. You might try budesonide MMX, beclometasone dipropionate (Clipper) or rectal steroids. If you’re having a severe flare-up you may need standard oral steroids.
Acute Severe Ulcerative Colitis (ASUC) is a serious condition. If you have ASUC, you’ll usually be treated with intravenous steroids in hospital. Intravenous steroids work quickly, so you should start to feel better within a few days. If you do not start to feel better, your IBD team will discuss other possible treatment options with you.
You may have oral budesonide to treat a flare-up of Microscopic Colitis. Sometimes you can have it longer term, to keep your symptoms under control. Microscopic Colitis includes Collagenous Colitis and Lymphocytic Colitis.
There are lots of things to think about when you start a new treatment. Your IBD team will discuss your options with you. When thinking about a new treatment you might want to consider the potential benefits, possible risks and the goals of your treatment. Some things to think about include:
Our Appointment guide has a list of questions you might want to ask. It can help you focus on what matters most to you. You might find our information about other medicines and surgery for Colitis helpful.
Use this tool to understand more about potential treatment options that suit your needs. The tool is designed to help you:
Steroids work well to reduce and control symptoms during a flare-up of Crohn’s or Colitis.
Find out more about how we talk about the effectiveness of medicines.
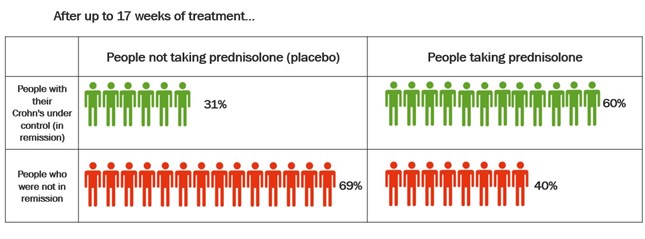
Two major studies have looked at how well steroids work in Crohn’s. The studies compared a total of 267 people taking either prednisolone or placebo. A placebo is a dummy treatment that looks the same but doesn’t have any medicine in it. The studies looked at how many people had their Crohn’s under control after up to 17 weeks of treatment. The table below shows the combined results of the studies.
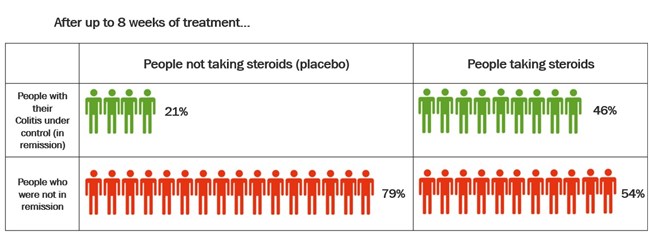
One review combined the results of five studies on Ulcerative Colitis. The studies compared different types of steroids with placebo (dummy treatment). The table below shows how well steroids got Colitis under control after up to 8 weeks of treatment.
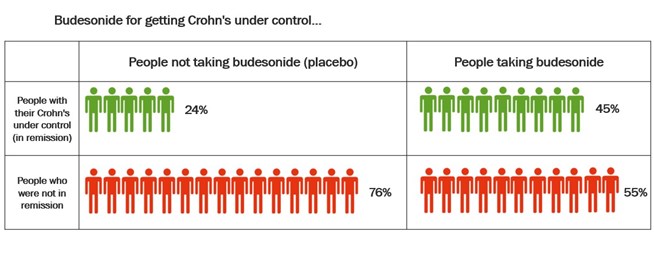
Budesonide is not as good at treating flare-ups as standard oral steroids. But because it acts directly on the affected area of your bowel, it causes fewer side effects. This means it is often preferred for mild flare-ups of Crohn’s or Colitis.
Several studies have compared budesonide to placebo for getting Crohn’s disease under control. The table below shows the combined results of all these studies.
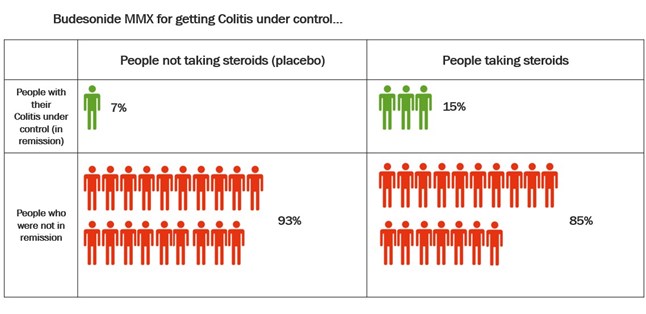
 Studies have also compared budesonide MMX with placebo in the treatment of Ulcerative Colitis. Budesonide-MMX designed so that the budesonide is not released until it reaches the colon. This means it can be useful in the treatment of Colitis. The table below shows the results of these studies.
Studies have also compared budesonide MMX with placebo in the treatment of Ulcerative Colitis. Budesonide-MMX designed so that the budesonide is not released until it reaches the colon. This means it can be useful in the treatment of Colitis. The table below shows the results of these studies.
It usually takes between 1 and 4 weeks for oral steroids to start working. In some people they work sooner than this and in others they can take more time to work. If you’re taking rectal steroids, your symptoms may start to get better within a week or two. If you’re taking intravenous steroids, you’ll usually start to feel better after a few days, but it can take longer.
You may experience side effects from steroids much sooner. See the section on Side effects for more information.
Steroids don’t work for everyone. Up to 1 in 3 people do not respond to steroid treatment at all. This is known as being steroid refractory. Some people have a partial response. This means that their symptoms improve but are not completely under control. Speak to your IBD team if your condition isn’t improving.
How you take steroids will depend on how severe your Crohn’s or Colitis is, and which part of your gut is affected.
These are steroid tablets, capsules, granules, dissolvable tablets or solutions that you swallow. The patient information leaflet that comes with your steroids will tell you how to take them. You will usually take oral steroids in the morning. You should take them with or just after food. Taking oral steroids in the morning can help reduce side effects.
The instructions may be different for delayed-released oral steroids. This includes budesonide or beclomethasone dipropionate (Clipper). You may need to take these before food in the morning. It’s important to swallow these medicines whole and not to chew, crush or break them. This may stop them from working.
This is an injection or infusion of a steroids into a vein. Intravenous steroids are used for severe flare-ups and can give the quickest response. You would only have intravenous steroids in hospital. You may then switch to oral steroids.
These are steroids that you insert into your bottom (rectum) with an enema or suppository. Enemas are liquids or foams, which you insert into your bottom with an applicator. Suppositories are small bullet-shaped capsules of medicine, which you place inside your bottom.
Read the instructions that come with your steroids. They’ll explain the best way to use them and often have pictures to help. In general:
Do not worry if you do not quite get it right the first few times, or if you spill some. It’ll soon become another part of your routine. If you are having difficulty using your medicine, talk to your IBD team.
The dose of steroid you’re prescribed will depend on the type of steroid and why you’re taking it. Your IBD team will advise you on this.
Typical doses for adults might be:
Do not make any changes to your dose or how you take your steroids without talking to your IBD team or GP.
Your doctor will prescribe as short a course of steroids as possible. This helps to control your symptoms and allows longer-term treatments to start to work. Taking steroids for a long time, or too often, will not help to control your Crohn’s or Colitis. It can also cause unwanted side effects. If you have been on steroids for 3 months or longer, talk to your IBD team about your treatment options.
It’s important to complete your full course of steroids. The length of a course of steroids is often about 8 weeks. But this will depend on the type of steroid you’re taking. It’s important not to suddenly stop taking steroids, even if you feel better. Depending on which type you have, your doctor may want to gradually reduce your dose. This is usually the case for prednisolone and budesonide. For more information see the section on Side effects.
After you have finished your course of steroids, your doctor may offer you a different treatment to keep your symptoms under control. This may be a 5-ASA, an immunosuppressant (such as azathioprine or mercaptopurine), a biologic medicine or a JAK inhibitor, such as filgotinib and tofacitinib. See our information on treatments for Crohn’s or Colitis. This may also be started while you are still taking the steroid.
Your doctor will want to limit how many steroids you have. If you need more than one course during a year, they may try other medicines to keep your condition under control. If your GP has prescribed you a course of steroids, they should let your IBD team know.
Steroids are often taken alongside other medicines used to treat Crohn’s or Colitis. Your doctor might prescribe them in combination with 5-ASAs or immunosuppressants to help control a flare-up. Or you might have a short course of steroids while taking your usual Crohn’s or Colitis medicines. Your IBD team will consider all your medicines when prescribing steroids.
You will need some checks before you start treatment with steroids to make sure they’re right for you. Let your IBD team know if you have:
And tell your IBD team if you:
As you’ll usually only be taking steroids for a short amount of time, you may not see your IBD team during this period. Contact your IBD team if you have any side effects or if steroid treatment is not working for you.
Your doctor may want to check for signs of weak bones (osteoporosis). See more on this in protecting your bones.
If you need to take steroids longer-term, your doctor will also check for a serious disorder called adrenal suppression. For more information on this, see the section on Side effects.
Taking steroids can weaken your bones. Taking them for a long period of time (more than 3 months), puts you at higher risk. If you’re having a longer course of steroids, your doctor will usually give you vitamin D and calcium supplements. This will help protect your bones and keep them strong.
Your doctor should assess your risk of bone fractures when you start taking steroids. They may suggest you have a bone density scan (also known as a DEXA scan).
If you are taking steroids for longer than 3 months, you should have a DEXA scan. Tell your doctor or IBD team if you haven’t had one and think you need to.
If you’re at high risk of bone fractures, your doctor will recommend you take a type of medicine called a bisphosphonate. This can help keep your bones strong. If you’re pregnant, or trying for a baby, let your doctor know. Bisphosphonate treatment may not be suitable for you.
Rectal steroids and budesonide are less likely to cause bone weakness than oral and intravenous steroids. This is because they work directly in your bowel and don’t tend to cause side effects in other parts of your body.
Other factors can increase the risk of developing weaker bones or osteoporosis. The Royal Osteoporosis Society has made a tool to check your risk of osteoporosis. You can use this tool to help you understand what might increase your chances of getting osteoporosis and broken bones. But, if you already know you have osteoporosis or have had your bones checked by a doctor, this tool is not for you. And it cannot tell you if you have osteoporosis. Note that this tool is not made specifically for people with Crohn’s or Colitis. And there are other factors related to your Crohn’s or Colitis can also make your risk of osteoporosis higher.
Keeping active and eating a balanced diet can help you maintain healthy bones. We have more about this in our information on Bones.
Carry a steroid card. Your pharmacist or doctor may give you a steroid card with details of your steroid treatment. This will include the dose and how long you’ll be taking steroids. Always carry this and show it to any healthcare professional treating you, even if it’s not related to your Crohn’s or Colitis. You could also consider wearing an emergency bracelet.
Speak to your doctor if you think you have an infection. Steroids affect the way your immune system works. This means your body might not be able to fight off infections as well as it usually does. Even a mild infection such as a cold or sore throat could develop into something more serious. Tell your doctor or IBD team if you feel unwell and think you might have an infection.
Avoid close contact with people who have infections. This includes chickenpox and shingles and measles. You could become seriously ill from these illnesses. Tell your doctor if you come into contact with anyone who has these infections.
Although steroids are produced naturally in your body, doses of steroid medicines are much higher. This can cause unwanted side effects. At least half of people taking steroids for Crohn’s and Colitis experience some side effects. Your doctor will try to reduce your risk by prescribing the lowest dose of steroids that works for you, and for the shortest possible time.
Rectal steroids (enemas and suppositories) and delayed-release oral steroids like budesonide cause fewer side effects than standard oral steroids. This is because they target the inflamed area and do not affect the rest of the body.
Some of the side effects that you might experience while taking steroids include:
Remember, not everyone will get side effects. And if you do, they are likely to be temporary and go away once you finish treatment. Some side effects may be more serious and need treatment. Speak to your IBD team if you experience any side effects. They can give you advice on how to manage them.
Do not suddenly stop taking steroids
If you’re taking oral steroids, it’s very important not to miss a dose, or to stop taking them suddenly.
For many oral steroid medicines, your body stops making enough of your own steroids while you’re taking them. This is known as adrenal suppression. You might not notice any problems while you’re still taking steroid medication. But suddenly stopping your medicines means your body won’t have had time to make its own steroids. You may develop symptoms of adrenal suppression, including:
Gradually reducing your steroid dose gives your body time to start making its own steroids. Your IBD team will guide you if you need to do this.
Sometimes reducing the dose of steroids can make your Crohn’s and Colitis symptoms come back. If this happens, you’ll be offered other medicines, to help you come off steroids completely.
Children may also have steroids to help control a flare-up of Crohn’s or Colitis. Doses of steroid are different for children. Doctors work this out depending on your child’s weight.
If your child is having a short course of steroids, they’re unlikely to get many side effects. The most common ones include:
Steroids can affect growth in children. This is usually only a problem for children taking long courses of steroids. If your child is taking steroids for a long time, your doctor will monitor their height and weight to check they’re staying on track.
There are some other points to be aware of if your child is taking steroids.
Talk to your child’s doctor about possible alternative treatments. Children may be able to have budesonide instead of a standard steroid for a mild Crohn’s flare-up. This often has fewer side effects. Children with Crohn’s can also have enteral nutrition as an alternative to steroids. See the section on Alternatives to steroids for more information.
Budesonide MMX (a controlled-release formulation of budesonide) is only recommended for adults. This isn’t available for children with Ulcerative Colitis.
Certain medicines can interact with steroids. This means it can affect how well the medicines work, or the risk of side effects. Talk to your doctor or pharmacist if you’re taking or plan to take any other medicines. This includes medicines that you buy from a pharmacy or a supermarket. It also includes any herbal, complementary or alternative therapies.
Common medicines that interact with steroids include:
NSAIDs are not usually advised if you have Crohn’s or Colitis, especially during a flare-up. They increase the risk of stomach ulcers and internal bleeding. This risk is even greater if you take NSAIDs while you’re also taking steroids. If you do need to take both, your doctor may recommend you also take another medicine called a proton pump inhibitor. This helps to protect your stomach and reduce the risk of these problems.
It’s fine to drink alcohol while you’re taking steroids. But try not to overdo it. Heavy drinking will increase your risk of developing stomach problems. To keep the health risks from drinking alcohol low it is best to stay within the recommended limits.
It’s not safe to have ‘live’ vaccines while taking steroids at the doses used for Crohn’s and Colitis. This is because steroids weaken your immune system, so you may be more likely to develop a serious infection. You’ll need to wait 3 months after you stop taking steroids before having a live vaccine.
Speak to your IBD team to make sure your vaccinations are up to date before you start taking steroids. If you have recently had a live vaccine, you should wait at least 4 weeks before starting steroids.
In the UK, live vaccines include:
The annual flu jab and pneumococcal and COVID-19 vaccines are not live vaccines and are safe to have while taking steroids.
If someone you live with is due to have a live vaccine, ask your IBD team if you need to take any special precautions.
There’s no evidence that steroids affect your ability to get pregnant.
It’s important to make sure your Crohn’s or Colitis is under control before trying for a baby. Having an active flare-up while you are pregnant is linked with various problems. It increases the risk of your baby being smaller than normal in the womb, being born early and having a low birthweight.
You can take steroids to control a Crohn’s or Colitis flare-up during pregnancy. Some research suggests that taking steroids when pregnant may also be linked with problems such as premature birth and lower birthweight. But we can’t be sure whether that’s due to the steroids or the condition itself.
Some small studies have shown a link between steroid use and risk of babies born with cleft lip and palate. But the evidence is mixed, and more recent larger studies have not found a link.
In general, the benefits of taking steroids during pregnancy are considered to outweigh any potential risks. Risks are higher if you take steroids repeatedly while pregnant, or for a long time. Your doctor will make sure you take them for the shortest possible time to get your disease back under control.
Budesonide is sometimes considered safer to take during pregnancy. This is because not so much of the medicine reaches the baby. There hasn’t been much research into taking budesonide during pregnancy. But two small studies of budesonide and budesonide MMX did not find any negative effects in mothers or babies.
Talk to your doctor before you start trying for a baby. They can make sure that your condition is under control. This will keep the chances of you needing to take steroids during pregnancy low. If you take steroids during pregnancy, make sure you tell the healthcare team involved in your baby’s birth.
It’s usually safe to breastfeed while taking steroids. Steroids may pass to the baby in your milk, but it’s a very small amount. If you are thinking about breastfeeding and you are taking a high dose of steroids (over 40mg prednisolone daily), check with your IBD team or your baby’s healthcare team first.
Enteral nutrition is a special liquid diet that you have instead of food. It’s an effective alternative to steroids for children with Crohn’s. Your child’s doctor may suggest it if there are concerns about steroids affecting their growth. Enteral nutrition doesn’t seem to be as effective as steroids in adults with Crohn’s. But you may want to consider it if you don’t get on with steroids or you’d prefer to avoid them. Speak to your IBD team if you want to find out more about enteral nutrition.
If you have severe Crohn’s and steroids and other medicines aren’t helping, you may be offered a biologic medicine instead. A biologic medicine may also be an option if you cannot take steroids for some reason, or you do not get on with them. Biologic medicines include infliximab and adalimumab.
You will usually only be offered steroids for Ulcerative Colitis if topical or oral 5-ASAs are not enough on their own.
If you have moderate to severe Colitis, and steroids and other medicines are not helping, you may be offered alternative medicines. These include biologic medicines and JAK inhibitors, such as filgotinib, tofacitinib or upadacitinib. These may also be options if you can’t take steroids for some reason, or you do not get on with them.
If you’re being treated for severe Colitis in hospital, you’ll usually be offered intravenous steroids first. But alternatives include intravenous ciclosporin, surgery and infliximab.
Your doctor will suggest stopping smoking and any medicines that could be making your symptoms worse. Budesonide is usually the first medicine that doctors prescribe for Microscopic Colitis. But if you cannot, or do not want to take steroids, they may suggest medicines for diarrhoea (such as loperamide) instead. See our information on Microscopic Colitis for details.
Always speak to your IBD nurse if you have any concerns or side effects. They see lots of people with IBD and have lots of valuable experience.
Barry
Living with Crohn's Colitis
Taking different medicines and managing side effects can be difficult – we understand and we’re here to help. Our Helpline can answer general questions about different treatment options and can help you find support from others with the conditions.
Your IBD team is also there to help you. You can talk to them about your steroid dosage, how they’ll be monitoring you and what alternatives may be available. You should also get in touch with your IBD team if you have any new symptoms or side effects.
It can take time to find the medicine that’s right for you. Don’t be afraid to ask questions and seek out extra support when you need it.
This information on steroids is general and doesn’t replace specific advice from your doctor or any other health professional. Talk to your GP or IBD team for information specific to you. You can also check the Patient Information Leaflet that comes with your medicine or go to medicines.org.uk/emc.
We follow strict processes to make sure our information is based on up-to-date evidence and easy to understand.
Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishop Square, Hatfield, AL10 9NE, or contact us through our Helpline: 0300 222 5700
Symptoms
Read information
Treatments
Read information
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
