Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last updated: April 2025
Last full review: February 2023
Next review date: February 2026
If you have Crohn’s or Colitis, what you eat may affect your symptoms. But it is different for everybody. This information aims to help you eat well with Crohn’s or Colitis and make informed choices about your diet.
This information might use words you have not heard before. Our page on medical words can help provide an explanation.
The Welsh Value in Health Centre has funded the development of this video as part of its Person Centred Care portfolio in collaboration with the IBD Wales group. You can find a Welsh version of this video here.

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Your gut is a long tube that starts at your mouth and ends at your bottom. It breaks down food so your body can get energy and nutrients from it. This is called digestion. Muscles in the walls of your gut squeeze the food along in a wave-like movement.
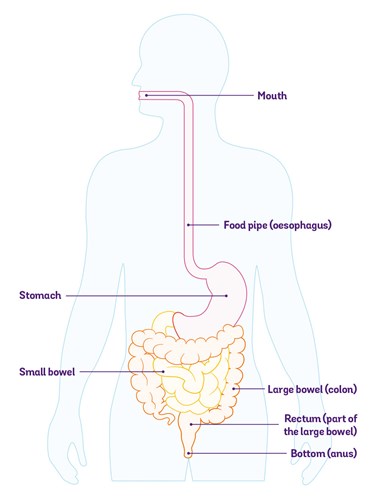
When you eat, food travels down your food pipe into your stomach. Your stomach makes acid, which kills germs. It also churns the food into a porridge-like consistency. The food then passes into your small bowel.
Your small bowel breaks down the food and absorbs energy and nutrients from it. Anything that is not absorbed is squeezed along to your large bowel.
Your large bowel absorbs liquid from the food. This usually leaves solid waste – poo.
Your body stores poo in a part of your large bowel called your rectum until you go to the toilet.
It usually takes around 1 to 4 days for food to pass all the way through your gut. But this can vary a lot from day-to-day, from person-to-person and depending on what you have eaten.
Crohn’s and Colitis cause inflammation in your gut.
If your small bowel is inflamed, you might not absorb nutrients or liquids as well as usual. So if you have Crohn’s, you might find it hard to get all the energy your body needs. You might also have low levels of some vitamins and minerals. If your large bowel is inflamed, you are likely to absorb most nutrients but you might not absorb enough liquid from your food or drink.
When you’re feeling unwell, it can also be difficult to eat enough of the right nutrients to stay well and keep a healthy weight. You might not feel like eating much, or you might only be able to tolerate certain foods. You may have a low appetite or lose weight without trying to. Some people might gain weight. This could be because of changes to your diet, or as a result of some treatments for Crohn’s or Colitis, such as steroids.
Many people with Crohn’s or Colitis change what they eat to try to help manage their condition. This can make it hard to get the right balance of nutrients. It can also change your relationship with food.
Food is such an important and joyful part of life, it’s a huge part of how we socialise in the UK. Sometimes it’s frustrating and sad not to be able to embrace that fully, especially when you’re flaring or recovering from a flare-up.
Indigo
Living with Crohn's
Many people say they do not get as much pleasure from eating as they used to. Changing your diet can also affect your family life, especially if you do not eat the same food as other people you live with. Up to 1 in 4 people with Crohn’s or Colitis say they avoid eating out or social events that involve food. This can be especially hard if food is a big part of your culture. You might feel excluded, or guilty for turning down food that has been offered to you. Some people find that taking a prepared meal from home can be helpful if they’re going to a community event where there might be food they can’t eat.
Many individuals find it helpful to learn more about diet and nutrition. They have told us that making informed food choices has had a positive effect on their overall health
There is no evidence that any particular food causes Crohn’s or Colitis. There’s nothing you could have done differently that would have prevented you from developing it.
We don’t know exactly what causes Crohn’s and Colitis. It is probably a combination of:

The food you eat can affect your health in lots of ways. It is a complicated relationship. Food can have direct effects on the lining of your gut. It can affect your immune system. It can also change the balance between helpful bacteria and harmful bacteria that live in your gut. So what you eat might affect your risk of getting Crohn’s or Colitis, but there is not enough evidence yet to say for certain.
Most people living with Crohn’s or Colitis feel that certain foods can trigger flare-ups. But so far, there is very little scientific evidence to prove this. Researchers are looking into it to try to find out more about how diet affects flare-ups.
Some people find that what they eat has little effect on their symptoms. Others find that certain foods trigger symptoms and cutting down on those foods helps. In some cultures, making and eating spicy food is common. Some people with Crohn’s or Colitis may find that eating spicy food makes their symptoms worse.
You could use a food diary or app to find out if any foods seem to affect your symptoms. If you find any possible triggers, it’s a good idea to discuss them with your IBD team or dietitian before making any big changes to your diet.
It is important not to cut foods out of your diet without talking to your dietitian or IBD team. It could mean you miss out on nutrients that your body needs.
Changes in symptoms after eating certain foods may not mean that your Crohn’s or Colitis is active or flaring up. Food can sometimes trigger symptoms in people without Crohn’s or Colitis too.
Learning what my triggers are, balancing my diet, managing my stress and keeping exercising have helped me.
Fiona
Living with Colitis
When your Crohn’s or Colitis is active, it can be hard to work out if a particular food is a trigger or if you’re getting symptoms because you’re in a flare-up. It may be easier to identify possible trigger foods when your symptoms are under control.
There is no evidence that following a particular diet can cure Crohn’s or Colitis.
You might hear about people who manage their Crohn’s or Colitis through diet alone, or diets that claim to cure Crohn’s or Colitis. But there is no evidence that these work. And they often restrict particular foods or food groups, so if you follow them for a long time, you may miss out on important nutrients.
However, there are effective nutritional treatments that are sometimes prescribed to treat Crohn’s.
Researchers agree that diet is important in Crohn’s and Colitis. But at the moment, there is not much high-quality evidence to say exactly what foods could be helpful and what foods could be harmful. It is also something that may vary a lot from person-to-person. Some people find that certain foods make their symptoms worse. The same foods might not cause any problems for another person. So there is not any particular diet that works for everyone.
There might be times when your IBD team recommend making other changes to you diet. This could happen if:
For me diet and lifestyle are key factors in staying well. But they aren't easy to prescribe like medication, and big changes are very hard for people to implement.
Sue
Living with Crohn's
What we eat varies a lot depending on our age, where we live, our cultural background, how active we are – and what we like. What one person thinks of as a ‘normal diet’ might not be the same for someone else. This can make it hard to work out the impact of diet on health conditions.
Food research often uses questionnaires to find out what the people taking part have eaten. But it’s hard to keep a record of exactly what you eat because every meal contains so many different ingredients. It can also be difficult to remember everything you’ve eaten, especially if the questionnaire covers a long period of time. And unless you weigh all your food, you will not know exactly how much of everything you’ve had. Even if two people record having the same meal, they might have used different ingredients, different brands or different cooking methods. All these things make it very difficult to prove whether particular foods do, or do not, help people with Crohn’s or Colitis.
If you have Crohn’s or Colitis, it can be difficult to eat a healthy, balanced diet. This means you have a higher risk of malnutrition than other people. Malnutrition is when you do not get the right amount of energy or nutrients. It can mean that you are not getting enough, you are getting too much, or you are getting the wrong balance of energy or nutrients. Malnutrition can make it harder for your body to heal and fight off infections.
You might find it hard to eat well when you’re in a flare-up. But when your condition is under control, eating a healthy, varied diet helps you get the right balance of energy and nutrients. This is good for all aspects of your health, not just your Crohn’s or Colitis.
I’ve struggled with the contradictions of trying to live a healthy life but not being able to eat healthy foods at times.
Indigo
Living with Crohn's
The Eatwell Guide is a useful starting point. It shows how much of each of the different food types you should aim to have in your diet. It is based on everything you eat and drink over a whole day – not necessarily in each meal.
Search ‘Eatwell Guide’ at www.nhs.uk or www.gov.uk for more about the Eatwell Guide.
I monitored my food intake closely and realised the trigger foods. I cut meat out of my diet and stopped drinking beer and wine.
Melanie
Living with Crohn's
It is recommended that people try to eat at least five portions of a variety of fruit and vegetables every day.
Fruit and vegetables should make up more than a third of the food you eat. They can be fresh, frozen, dried or canned. They’re a good source of vitamins, minerals and fibre.
Ask your GP, IBD team or dietitian for advice if you have problems eating fruit and vegetables, for example, if you have a stricture. Vegetables that are peeled and well-cooked can be easier to digest.
Base your meals on starchy foods if you can.
These should make up over a third of the food you eat. They give you energy and nutrients. Starchy foods include:
Choose wholegrain or wholewheat options and leave the skin on potatoes if you can – they contain more fibre.
As part of a balanced diet, it is recommended that you eat some beans, pulses, fish, eggs, meat and other proteins. If you eat fish, aim to have two portions a week. This includes one portion of oily fish.
Your body needs protein to grow and repair itself. Protein-rich foods also contain vitamins and minerals.
Try to eat less red meat, fatty meat or processed meat, like sausages, bacon or cured meats. Beans, peas, chickpeas and lentils are healthy alternatives. Tofu, bean curd and mycoprotein (Quorn) are also good sources of protein.
Fibre is a type of carbohydrate found in plants. It helps keep your bowel working by softening and bulking up your poo. Guidelines recommend that you eat 30g of fibre a day. But most people with Crohn’s or Colitis have a low intake of fibre. Some people feel that it makes their symptoms worse, so they might avoid it. Current guidelines say that unless you have a narrowing (stricture) in your gut, there is no need to limit your fibre intake when your condition is under control.
Fibre-rich foods include:
Some people find it hard to eat enough fibre during a flare-up, but when you start to feel better, it’s important to get back to eating a healthy, balanced diet.
Have some dairy or dairy alternatives.
Dairy foods are good sources of proteins, vitamins and minerals – especially calcium. They include milk, cheese, paneer, yoghurt and fromage frais. Go for lower-sugar products if you can.
Dairy alternatives include soy, oat or nut milks. If you use dairy alternatives, try to make sure they are unsweetened and have added calcium. These are sometimes called fortified drinks.
Eat small amounts of unsaturated oils and spreads.
Oils and spreads are fats. They are high in energy so you only need small amounts. Most people have too much fat in their diets.
There are different types of fat, and some are healthier than others. Unsaturated fats like olive oil, fish oils or nut oils are healthier than saturated fats like butter, ghee or lard. Choose lower-fat versions if you can. Vegetable fats are healthier than animal fats.
The British Heart Foundation has more information on different types of fat. Search ‘fats’ at www.bhf.org.uk
If you choose foods and drinks that are high in fat, salt or sugar, try to have them less often and in small amounts.
Foods or drink high in fat, salt or sugar include:
Butter, ghee, palm oil and coconut oil are also high in fat, sugar or salt.15
You do not usually need these foods or drinks in your diet, but it’s OK to have them occasionally and in small amounts. If you eat them a lot, cut down if you can, especially if you are above a healthy weight.
Aim to drink 6 to 8 cups or glasses of fluid a day.
This could be water, tea, coffee, lower-fat milk or sugar-free drinks. Fruit juice and smoothies also count but they are high in sugars. When you are well, you should try to limit juice or smoothies to one small glass per day.
There is not enough high-quality evidence to know for certain if drinking alcohol could increase your risk of a flare-up. But many people with Crohn’s or Colitis say that alcohol makes their symptoms worse.
If you drink alcohol, try to keep to the recommended limits.
Visit www.drinkaware.co.uk for more information about low risk drinking guidelines.
It can be difficult to find reliable information about food for people with Crohn’s or Colitis, and some of the information you get can be conflicting. Many people use ‘trial and error’ to try to work out what foods to eat and what to avoid, but this may not work well and it can lead to missing out on important nutrients. Be careful with information about diet you find on the internet. It may not be reliable and it could be dangerous.
If you’re not sure where to find trustworthy information, you could ask your GP or IBD team for recommendations. Some may be more knowledgeable about the role of diet than others.
You could also contact Crohn’s & Colitis UK or the other organisations listed at the end of this page.
Your GP or IBD team might be able to refer you to an NHS dietitian. Some people choose to contact a private dietitian. If you cannot get an appointment with a dietitian, your IBD team may be able to give you information about diet.
Search ‘find a dietitian’ at www.bda.uk.com to find a private dietitian registered with the Association of UK Dietitians.
If you’re in a Crohn’s flare-up, you’re struggling to get enough nutrients from your diet or your bowel is not working, you might need nutritional treatments.
Nutritional treatments give you the energy and nutrients your body needs. There are two main ways to have them:
Enteral nutrition is a liquid diet. It comes as a ready-made drink or a powder that you mix with water. You can drink it, or you can have it through a feeding tube that goes straight into your gut. It is nutritionally balanced and gives you the energy and nutrients your body needs.
Depending on why you need it, you might have enteral nutrition instead of eating food. This is called exclusive enteral nutrition. Or you might have it alongside other food and drink. This is called partial enteral nutrition.
Exclusive enteral nutrition is a liquid-only diet. It is sometimes used to treat Crohn’s, particularly in children. It is not helpful for people with Ulcerative Colitis. It might sometimes be used if you have a severe flare-up, or if you’re having surgery for Crohn’s.
Exclusive enteral nutrition is often the first-choice treatment for children with Crohn’s. It works as well as steroids at getting Crohn’s under control. It also improves growth and nutrition in children with Crohn’s.
In adults, exclusive enteral nutrition does not seem to be as good as steroids at getting Crohn’s under control. But this might be because it is harder to follow a course of exclusive enteral nutrition so some people stop taking it. It can be helpful for people who cannot take steroids, or who do not want to take steroids. You might have it alongside immunosuppressant or biologic medicines. Some people might have it before surgery.
I had a liquid meal replacement to reduce inflammation before surgery to remove 30cms of small intestine. I replaced all meals over 10 weeks, up to the date of my surgery.
Lynda
Living with Crohn's
If you’re struggling to get enough energy or nutrients in your diet, you might have enteral nutrition alongside normal food and drink. This is called partial enteral nutrition. For people with Crohn’s, having partial enteral nutrition as well as your usual medicines might help keep your condition under control.
I often feel tired and nauseous and can’t always eat solids so take a supplement drink to help with nutrition.
Akua
Living with Crohn's
For children with Crohn’s, partial enteral nutrition is sometimes used on its own or alongside medicines to help keep the condition under control for as long as possible. Or it might be used temporarily to help keep Crohn’s under control while other medicines take effect.
Parenteral nutrition delivers energy and nutrients straight into your bloodstream through a tube in a vein in your chest, arm or neck. This means it bypasses your gut completely. You might have it if you cannot absorb enough nutrients through your gut. Most people with Crohn’s or Colitis do not need it.
You might have parenteral nutrition if:
You usually have parenteral nutrition in hospital. If you need it, your IBD team or dietitian will explain how it will work and how long you’ll need it for. Very occasionally, if you need it in the longer term, your IBD team might arrange for you to have it at home.
When you’re in a flare-up, you might not feel like eating much. But it is still important to get enough energy and nutrients. You might find it helps to:
When you start to feel better, it’s important to get back to eating a healthy, balanced diet. If certain foods made your symptoms worse during your flare-up, try adding them back in to your diet gradually when you’re well.
If your symptoms are always active and you find it hard to eat a healthy diet, ask if you can be referred to a dietitian for support.
If you have a stricture (a narrowing in your gut), you may need to change what you eat to help prevent a blockage.
You might be advised to avoid foods that could block your gut, such as:
Try to eat sources of fibre that are easy to digest, like well-cooked, peeled vegetables, bananas, melons, or fruit juice. Drinking plenty of fluid at mealtimes is also helpful.
If you’re not able to get enough energy or nutrients in your diet, you may need to have nutritional treatments.
Diarrhoea is a common symptom of Crohn’s and Colitis. Some people find that food has no effect on their diarrhoea. Others find that avoiding certain foods helps. You could use a food diary or app to find out if any foods seem to affect your symptoms.
Foods or drinks that might make diarrhoea worse in people with or without Crohn’s or Colitis include:
It is important to make sure you drink plenty of fluids to avoid dehydration.
We have more information about diarrhoea.
Some people with Crohn’s or Colitis get constipated. This might be caused by the condition itself, medicines you’re taking, or difficulty eating and drinking.
If you’re constipated, changing your diet can help. But it may take a few days or even a few weeks to work. You could try:
We have more information about constipation.
If you have Crohn’s or Colitis, you might feel bloated and gassy. Your tummy might make loud noises, or you might fart more than usual. It might be painful. Keeping a food diary can help you find out if any foods make your symptoms worse. Wind is not necessarily a bad thing, but if it is causing you problems, you might find it helpful to:
If you have irritable bowel symptoms as well as Crohn’s or Colitis, you may find that a low FODMAP diet helps reduce bloating and wind.
You might get dehydrated if you’re not able to drink enough, or if your body is losing lots of fluid. This can happen if you have frequent diarrhoea, you’re being sick or you have a high-output stoma.
If you think you’re dehydrated, you could try:
Contact your IBD team if you think you are dehydrated and you have:
Some people with Crohn’s or Colitis feel sick and may be sick. Some medicines for Crohn’s and Colitis can also cause sickness. Here are some things that may help:
Many people with Crohn’s or Colitis experience fatigue – extreme tiredness that does not go away when you rest.
Not having enough energy or nutrients in your diet is one of the things that can cause fatigue. If you have low levels of particular nutrients, taking the right supplements may help your fatigue. It’s also important to try to eat a diet that contains all the nutrients you need. But this can be difficult when your energy levels are low.
When your fatigue is bad, you may not have enough energy to cook or even to eat much. It can help to choose foods you enjoy. You could also ask friends or family to help with shopping and cooking. During times when you have more energy, you could batch-cook meals for a few days so you have food ready for days when your energy levels are low.
We have more information about fatigue.
Some people with Crohn’s and Colitis have other medical conditions that may involve changes in diet. Here, we cover some of the more common ones. This is an overview of how diet may help – we do not cover medical treatments for these conditions.
Sometimes, you might get conflicting dietary advice for different conditions. If you have complicated dietary needs, you might be referred to a dietitian.
Irritable bowel syndrome (IBS) is an illness that causes gut symptoms but does not show any signs of damage to the gut on tests. It can cause symptoms like cramping tummy pain, bloating and wind, diarrhoea or constipation. Around 10 in 100 people in the general population have IBS.
I’ve been living with Crohn’s disease for a decade now. And I was diagnosed with IBS a few years previously. But I’m still really unsure how to tell the difference between the two. Is it Crohn’s or IBS that’s causing the painful bloat and constipation? Is it Crohn’s or IBS that dislikes dairy, wheat, red meat and fatty foods?
Franchesca
Living with Crohn's
IBS, or IBS-like symptoms, affect more than 30 in 100 people with Crohn’s or Colitis. This means you might have gut symptoms even if your Crohn’s or Colitis is under control (in remission).
If you have IBS (or IBS-like symptoms) and Crohn’s or Colitis, following a low FODMAP diet might help you identify possible trigger foods. But it is not designed to be followed long-term. If you follow a low FODMAP diet, you should be supervised by a trained dietitian.
Gluten is a protein found in wheat, barley, rye, or foods that contain them. This includes bread, breakfast cereals, pasta, cakes and many other shop-bought foods. There is no evidence to suggest that gluten is bad for Crohn’s or Colitis. But some people with Crohn’s or Colitis might also have coeliac disease or gluten sensitivity.
Coeliac disease is a condition where your immune system attacks the lining of your gut if you eat gluten. It causes symptoms similar to Crohn’s and Colitis, like diarrhoea, tummy pain, bloating and wind.
Some people do not have coeliac disease but get symptoms when they eat foods containing gluten. This is called gluten sensitivity. Scientists are not sure what causes gluten sensitivity. They think it might not be gluten that causes the problem, but other components of wheat, barley or rye.
In the UK, fewer than 1 in 100 people have coeliac disease. But around 13 in 100 think they are sensitive to gluten. This is higher in people who have Crohn’s or Colitis – around 25 in 100 people with Crohn’s or Colitis say they are sensitive to gluten. This can happen temporarily during a flare-up.
If you think you have coeliac disease or gluten sensitivity, speak to your IBD team or dietitian before changing your diet. It’s important to get a diagnosis so you can get the right monitoring and treatment. The tests for coeliac disease only work properly if you are eating gluten.
The treatment for coeliac disease is a gluten-free diet.
If you cut gluten out of your diet during a flare-up, try adding it back in to your diet gradually when you’re well.
Coeliac UK provides information and support for people with coeliac disease at coeliac.org.uk
Lactose is a sugar found in dairy products, like milk, cream and cheese. An enzyme called lactase in the lining of your small bowel usually breaks it down so your body can absorb it. Babies usually have high levels of lactase, but older children and adults may not make enough lactase.
If lactose is not broken down, your body cannot absorb it. This is called lactose malabsorption. It might not cause any problems at all. But it can cause symptoms like diarrhoea, bloating, wind, tummy pain and feeling sick. If it causes symptoms, it’s called lactose intolerance.
In the UK, around 8 in every 100 people are lactose intolerant. People with Ulcerative Colitis have a similar risk of being lactose intolerant as the general population. But people with Crohn’s may have a slightly higher risk. Some people with Crohn’s or Colitis only get symptoms of lactose intolerance during a flare-up.
Symptoms of lactose intolerance may be similar to flare-ups. So it’s important to talk to your IBD team before cutting out lactose.
If you have Crohn’s or Colitis and lactose intolerance, cutting down on foods and drinks that contain lactose might help reduce the symptoms. You could choose dairy alternatives with added calcium or look for lactose-free dairy products. Check the ingredients on foods you buy to see if they contain lactose.
You might not need to cut out lactose completely – many people with lactose intolerance can manage small amounts of milk, especially if they have it with food. Once your symptoms have settled, try introducing lactose again to see if you can tolerate it.
Milk and dairy foods are important sources of calcium and vitamin D. If you follow a low-lactose or lactose-free diet, try to choose dairy alternatives with added calcium. Lactose-free cow’s milk products are still rich in calcium. You could also include other sources of calcium. If you cannot tolerate any calcium-rich foods, consider taking a calcium supplement.
Allergy UK have more information about lactose intolerance at allergyuk.org/lactose
Diverticula are small bulges or pouches in the bowel wall. They are very common, especially in people over 60. Most people do not know they have them. They are usually found during tests for something else.
Your IBD team might see diverticula during a colonoscopy.
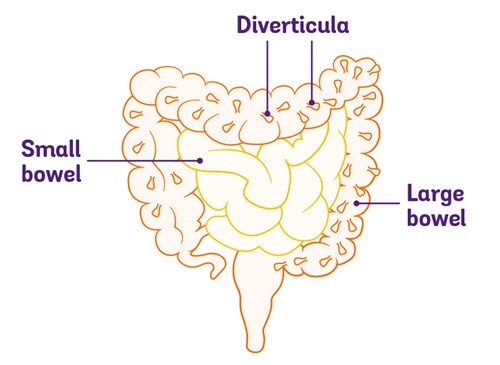
Most of the time, diverticula do not cause any symptoms. If you have diverticula but they do not cause any symptoms, it is called diverticulosis. If they do cause symptoms, it’s called diverticular disease. Sometimes, diverticula can get inflamed. This is called diverticulitis.
Symptoms of diverticular disease can be similar to Crohn’s and Colitis – tummy pain, bloating, diarrhoea or bloody poo. Diverticular disease can also cause inflammation in the bowel. So it is sometimes difficult to tell if you have diverticular disease or Crohn’s or Colitis. Around 1 in 10 people with Colitis might have diverticular disease as well.
If you have diverticular disease and Crohn’s or Colitis, a healthy, balanced diet that includes wholegrains, fruits and vegetables helps you get the energy and nutrients you need. Drinking plenty of water and regular physical activity can also help keep your bowel function regular.
Search ‘diverticular disease’ at gutscharity.org.uk for more about diverticular disease.
Some people with Crohn’s or Colitis may develop a difficult relationship with food. The effect of food on your symptoms can affect how you feel about eating. You may also have weight changes that you may find challenging. Some people lose weight, especially during a flare-up. Others might gain weight. This could be due to changes in your diet, medicines you’re taking, or the illness itself.
Eating disorders, like anorexia, bulimia or binge-eating disorders, are slightly more common in people with Crohn’s or Colitis than in other people. So some people might have an eating disorder as well as Crohn’s or Colitis. Avoiding particular foods or following diets that limit whole food groups can increase the risk of developing an eating disorder. They can sometimes cause similar symptoms to Crohn’s and Colitis, like tummy pain, weight loss and vomiting. Because of this, it can be difficult to get the right diagnosis.
It’s important to speak to your GP or IBD team if your weight is changing or you think you might have an eating disorder. They can offer support and refer you to specialist eating disorder services if needed.
For more information about eating disorders, visit Beat at beateatingdisorders.org.uk
People with Crohn’s or Colitis have a slightly higher risk than other people of developing heart disease. This may be partly due to long-term inflammation. If you have heart disease as well as Crohn’s or Colitis, a healthy, varied diet can help you stay as well as possible.
The British Heart Foundation has more information on heart disease at bhf.org.uk
People with Crohn’s or Colitis do not seem to be any more likely than other people to get diabetes. If you have diabetes and Crohn’s or Colitis, a healthy, varied diet helps you get the energy and nutrients you need. If you find it difficult to balance your diet for diabetes with your Crohn’s or Colitis, ask your team to refer you to a dietitian.
Visit diabetes.org.uk for more information about eating if you have diabetes.
People with Crohn’s or Colitis may not have enough vitamins or minerals in their body, or may not get the right amount of energy. This is called a nutritional deficiency. It might happen if:
Your IBD team should check if you have any nutritional deficiencies. This may include checking your height and weight, measuring your waist, hips or arms, checking how strong your grip is, and taking blood tests. They might also ask you about your diet.
Many people with Crohn’s or Colitis have undernutrition. This means your diet does not give you all the calories you need and you might lose weight without trying to.
If you are undernourished, your IBD team should refer you to a dietitian. They can give you specialist advice and support. It is important to treat undernutrition because it can make it harder to keep your Crohn’s or Colitis under control.
If you are not getting enough calories in your diet, you could try:
If this is not enough, your IBD team or dietitian might recommend enteral nutrition.
Just like everyone else, people with Crohn’s or Colitis can be any shape or size. Some people lose weight, but others might gain weight. Weight gain in Crohn’s or Colitis might be due to changes in your diet, medicines you’re taking, or the illness itself. Some people with Crohn’s or Colitis might be overweight or obese. But they still might not be getting enough of the right nutrients.
Eating a healthy, varied diet, together with regular exercise, can help you manage your weight and get the right balance of nutrients. But it’s better to wait until your Crohn’s or Colitis is under control before trying to lose weight.
Your body needs vitamins and minerals to work and stay healthy. Having Crohn’s or Colitis might stop you absorbing enough vitamins and minerals from your food. Or you might find it hard to get enough vitamins and minerals in your diet.
You are likely to have blood tests to check your vitamin and mineral levels. How often you need them depends on how well controlled your Crohn’s or Colitis is, whether you’ve had surgery, and whether you’re taking supplements.
If you think you might have a vitamin or mineral deficiency and you have not been offered blood tests, ask your GP or IBD team for them.
Eating a healthy, varied diet helps improve the balance of vitamins and minerals in your body. But if blood tests show you have low levels of particular vitamins or minerals, your GP, IBD team or dietitian might suggest you take supplements. You could choose to take a multivitamin, but this might not give you enough of the particular vitamins or minerals you’re low on.
Around 1 in 3 people with Crohn’s or Colitis have low iron levels. This could be because you’re not getting enough iron in your diet, you’re losing blood, or you have problems absorbing iron from food. Low iron levels can lead to anaemia, where you do not have as many red blood cells as you should to carry oxygen around your body. This can make you feel tired, breathless or dizzy.
I have iron-deficiency anaemia. This means I should increase my iron intake through vegetables. However, most of these are hard to digest due to me having a stricture.
Reece
Living with Crohn's
Anaemia caused by low iron levels is called iron-deficiency anaemia. If you have it, you’re likely to need iron supplements. You usually have these as tablets, capsules or liquid medicine that you take by mouth. But if you’re in a flare-up, your red blood cells are very low or you get bad side effects from oral iron supplements, you might have iron through a drip into a vein. This is called an iron infusion.
Your IBD team or dietitian might also check if you’re getting enough iron in your diet. If you’re not, you could try eating more iron-rich foods, like:
It’s harder to absorb iron from plant-based foods than from meat, but having some vitamin C at the same meal can help. For example, you could have a glass of orange juice with your fortified breakfast cereal.
Drinking tea or coffee with your meal – even decaf products – can make it harder for your body to absorb iron from your food. Try to wait an hour after eating before you drink tea or coffee.
Calcium and vitamin D help keep your bones and teeth healthy. But many people with Crohn’s or Colitis have low levels.
If your Crohn’s or Colitis is active, or you’re taking steroids, you should have a blood test to check your vitamin D levels. Blood tests are not helpful to check for low calcium levels, but your IBD team might check how much calcium you get in your diet instead.
You may need to take supplements if your calcium or vitamin D levels are low. Getting enough calcium and vitamin D is especially important for people who are going through menopause, or have already gone through it.
You can get calcium from dairy foods, fish with bones that you eat, broccoli, kale, spring greens and foods with added calcium, like breakfast cereal, bread and fortified plant-based dairy alternatives.
You can get vitamin D from eating oily fish, egg yolks, meat and foods with added vitamin D, like some breakfast cereals or yoghurts. But it’s hard to get enough from your diet in the winter. The Department of Health recommends that everyone over 1 year old – with or without Crohn’s or Colitis – should take 10 micrograms (10mcg) of vitamin D every day between September and March.
Some research has looked at whether vitamin D can help keep Crohn’s or Colitis under control. But there is not enough evidence to support this at the moment.
Your body uses folic acid and vitamin B12 to make red blood cells. If you do not have enough folic acid or vitamin B12, you may get anaemia. Folic acid is also called folate or vitamin B9.
If your folic acid or vitamin B12 levels are low, you may need to take supplements. You might have these as tablets, capsules or liquid medicine that you take by mouth. If you have anaemia due to low vitamin B12 levels, you are likely to have B12 as an injection.
You could also try to get more folic acid and vitamin B12 in your food.
Your IBD team, GP or dietitian might also check your levels of magnesium, potassium, zinc, phosphate, selenium and some vitamins.
Researchers agree that diet is important in Crohn’s or Colitis. There is a lot of research looking into diets that might be helpful. But at the moment, there is not enough evidence to recommend any particular diet for people with Crohn’s or Colitis.
We know that everyone is different and what works for one person may not work for another. It may take a while to find out what works for you.
I have quickly learned that managing my Crohn’s requires trial and error and balance. Especially with diet. Everyone is different and advice for one person may not work for another.
Reece
Living with Crohn's
Here, we cover some of the main diets that people ask about. Some people may find these diets helpful. But many of these diets are restrictive and they may lead to nutritional deficiencies if you follow them in the long-term.
If you decide to follow any diet to help with your Crohn’s or Colitis, it’s important to discuss it with your IBD team first. They may refer you to a dietitian. They can check that the diet is suitable for you and that you’re getting enough essential nutrients.
I've lost count of all the medications I've tried, the camera procedures, the amount of bloods I've had done, the diets I've tried.
Stephanie
Living with Colitis
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. These are carbohydrates that are hard to digest. When the undigested carbohydrates pass through the bowel, they attract water. This may cause diarrhoea. They also feed bacteria in your large bowel, which release gas. This can lead to bloating and wind.
A low FODMAP diet is a three-phase diet designed to identify possible trigger foods for IBS symptoms:
A low FODMAP diet cuts out a lot of foods during phase one. It is not designed to be followed long-term and it does not work for everyone. If you try a low FODMAP diet, you should do it with supervision and support from a trained dietitian.
A low FODMAP diet might be helpful for people with Crohn’s or Colitis that is under control or only mildly active, but who still have tummy symptoms. These might be tummy pain, bloating, wind, diarrhoea or constipation. At the moment, though, there is not enough high quality evidence to know for sure if a low FODMAP diet is effective. More research is going on.
The theory behind a high-fibre diet is that bacteria in your gut can convert fibre into substances that may help reduce inflammation. A high-fibre diet includes lots of foods like:
There is not enough evidence to know if a high-fibre diet is helpful for people with Crohn’s or Colitis. But fibre is important for your general health, and most people with Crohn’s or Colitis have a low intake. So if eating more fibre does not make your symptoms worse, there is no need to limit how much you eat unless you have a narrowing in your gut (a stricture).
A low-residue diet limits high-fibre foods that are hard to digest, like fruit and vegetable skins, nuts, seeds and wholegrains. It also limits foods that can stay in your bowel for a while, like milk. Some people try a low-residue diet to help reduce symptoms during a flare-up. But there is no high-quality evidence that it works.
Fibre is an important part of your diet, so if you choose to follow a low-residue diet during a flare-up, it’s important to gradually increase the amount of fibre you eat when you are better.
You may hear about other diets that some people with Crohn’s and Colitis follow. They may be helpful for some people but there has not been enough research done into their effects to say whether they work.
If you’re thinking about trying any of these diets, it’s a good idea to talk to your IBD team or dietitian first. They can check that the diet is suitable for you and that you’re getting enough essential nutrients.
The CDED involves taking liquid food alongside a diet that’s high in protein and low in animal fat, gluten and additives. Over time, you reduce the amount of liquid food you have and introduce restricted foods back into your diet. It might be helpful for some people with Crohn’s, but there is not enough evidence to recommend it at the moment.
The CD-TREAT diet aims to get as close as possible to exclusive enteral nutrition using ordinary food rather than a liquid diet. It is high in protein but cuts out gluten, lactose, alcohol and dietary fibre. You take a multivitamin as well.
The CD-TREAT diet seems promising for people with Crohn’s. But it is still being developed and there is not enough evidence to recommend it at the moment.
The specific carbohydrate diet is a low carbohydrate diet that limits:
The idea behind it is that people with Crohn’s or Colitis cannot absorb carbohydrates properly. So they pass into the large bowel, where bacteria feed on them. This may affect the balance of bacteria in your gut, which could impact your symptoms.
A specific carbohydrate diet might be helpful for some people with Crohn’s or Colitis. But there is not enough high-quality evidence to know for sure. A recent study found it was no better than a standard Mediterranean-style diet at getting Crohn’s under control and had no benefit on inflammatory markers. The diet can be difficult to follow because it limits a lot of foods.
The anti-inflammatory diet is loosely based on the specific carbohydrate diet but it does not limit as many foods. It includes probiotics and foods containing natural prebiotics to encourage gut-friendly bacteria and reduce inflammation. There has been very little research testing the diet in people with Crohn’s or Colitis. So there is not enough evidence to recommend it at the moment.
Gluten is a protein that’s found in wheat, barley, rye and oats, or foods that contain them. Around 1 in 4 people with Crohn’s or Colitis say they are sensitive to the effects of gluten and follow a gluten-free diet. This might improve symptoms for some people, but there is not enough evidence to recommend it for everyone with Crohn’s or Colitis. A gluten-free diet is also low in FODMAPs, so it could be FODMAPs rather than gluten that are causing problems.
A Mediterranean diet is high in fruit, vegetables, beans, pulses, cereals and healthy fats. It includes some fish and dairy products. It is low in meat and unhealthy fats.
It might be helpful for some people with Crohn’s or Colitis but there is not enough evidence to know for certain yet. There is a lot of research going on but at the moment, it is not conclusive. A Mediterranean diet is a healthy diet to follow and includes all the nutrients you need.
There is not enough high-quality evidence to know whether plant-based diets help get or keep Crohn’s or Colitis under control. But plant-based diets are generally healthy and are lower in fat and higher in fibre than meat-based diets. If you choose to follow a plant-based diet, try to make sure you get enough protein. You may also need to take supplements if you have any vitamin or mineral deficiencies.
I tried many different diets over the years to try and identify foods that were giving me problems and whilst becoming a vegetarian seemed to help, there were still times when I had no idea what was causing the problems.
Bill
Living with Crohn's
Some people take supplements or herbal remedies alongside medicines for Crohn’s or Colitis. But there is very little evidence that they help control symptoms.
If you want to take supplements or herbal remedies, it’s important to speak to your IBD team or dietitian first. Do not stop taking your prescribed medicines without talking to your IBD team, even if your symptoms improve.
Omega-3 is found in fish oils. Guidelines for people with Crohn’s or Colitis do not recommend taking omega-3 supplements because there is no evidence that they help.
Probiotics are foods or supplements containing friendly bacteria. You can buy them as drinks, yoghurts, tablets or powders. Fermented foods like kefir, kimchi, tempeh and kombucha are also probiotic.
There is no evidence that probiotics are helpful for people with Crohn’s. But, alongside prescribed medicines, they might help some people with mildly active Ulcerative Colitis get the condition under control. Some people might get side effects like diarrhoea or bloating. Probiotics might also be helpful for people who’ve had pouch surgery and have pouchitis.
There are lots of different probiotics, containing different bacteria. A type called VSL#3, which contains eight different strains of friendly bacteria, has been studied the most in Colitis.
Prebiotics are high-fibre foods or supplements that your body cannot digest well. Instead, they pass into your large bowel where they feed friendly bacteria. There is no high-quality evidence that prebiotics are helpful for people with Crohn’s or Colitis.
If you choose to try prebiotics, they seem to be safe to use alongside prescribed medicines. But they can make symptoms like bloating, diarrhoea and wind worse.
If you have active inflammation, your body uses more protein than usual, so you might think about using protein shakes. People might also consider taking protein supplements as part of an exercise programme. But there is not much evidence on the effect of protein supplements in people with Crohn’s or Colitis.
Protein supplements are highly processed and contain a lot of ingredients. Some of these might cause side effects if you take them for a long time. If you can, it’s better to get protein from food rather than supplements. This also helps you get other nutrients your body needs.
If you choose to use protein supplements, check the ingredients. Different supplements contain different sources of protein so choose one that’s suitable for you. It’s important to follow the instructions on the packet and mix the supplement with the right amount of water.
Some people try herbal remedies alongside prescribed medicines to help manage their symptoms. But there is not much high-quality evidence to say whether they work, or what is a safe dose. So they are not generally recommended for people with Crohn’s or Colitis.
If you decide to try herbal remedies, it’s important to tell your IBD team. Some herbal remedies can interact with prescribed medicines or cause serious side effects.
Some herbal remedies that you might hear about include:
You might have read that people with Crohn’s or Colitis should limit or avoid foods containing artificial sweeteners, thickeners, and other additives like carrageenan or titanium dioixide. This guidance is based on studies in animals. There is no high-quality evidence to say what effect additives have on people with Crohn’s or Colitis. But additives are not needed as part of a healthy diet. So if you choose to avoid them, you will not be missing out on any essential nutrients.
There might be special situations when you need to change what you eat. Here, we give a brief overview, with guidance on where you can find more information.
Having received my diagnoses, my focus was learning to live with all the new information presented to me, managing my meds and my diet.
Hakeem
Living with Crohn's
Most people are able to get back to eating a healthy, balanced diet after surgery for Crohn’s or Colitis. If you’ve had a lot of your bowel removed and you are not able to absorb enough water or nutrients, your dietitian will advise you on what to eat to stay well.
Most people who have a stoma can eat a healthy, balanced diet. But sometimes you might need to make some changes to what you eat.
We have more information on living with a stoma, including eating if you have an ileostomy or a colostomy.
If you’re pregnant or trying to get pregnant, it’s important to speak to your GP or IBD team to make sure you’re getting all the nutrients you need. It is also recommended that you take:
We have more information about pregnancy, including eating when you are pregnant.
Children and teenagers need more nutrients per kilogram of body weight than adults to help them grow. Your child’s IBD team will check whether your child is absorbing enough nutrients from their food. If not, they might recommend supplements. If your child has Crohn’s, their IBD team might recommend a liquid diet (exclusive enteral nutrition) for 6 to 8 weeks to get their condition under control.
Search ‘diet’ at www.cicra.org for more information about diet and nutrition in children with Crohn’s or Colitis.
If you are on medicines that lower your immune system, you might not be able to fight off infections as well as other people. To lower your risk of getting infections spread through food, it’s important to store and prepare food safely. And wash your hands before preparing or eating food.
Look for the latest Food Standards Agency’s consumer advice on food hygiene at www.food.gov.uk for more information on how to store and prepare food safely.
It’s important to speak to your dietitian or IBD team if you’re thinking about fasting for health or religious reasons.
There is very little evidence on the effect of intermittent fasting or time-restricted eating on Crohn’s or Colitis. Intermittent fasting for religious reasons, such as during Ramadan, does not usually cause problems for most people with Crohn’s or Colitis. But some people might find their symptoms get worse. Your IBD team might advise you not to fast if:
Up to 1 in 4 people with Crohn’s or Colitis say they avoid eating out because it is hard to control what food they’re eating. If you would like to eat out but you have particular dietary needs, let the restaurant know. It’s OK to ask about ingredients or how things are cooked. Some people find it helpful to explain that they do not have an allergy, but that some foods could trigger serious symptoms. You could contact restaurants beforehand to find out if they can meet your needs.
It can be really frustrating to not eat what food you want; it can make eating out really hard. I’ve now got ‘safe’ foods that I know I can fall back on, but planning is needed for eating out and travelling for me.
Kathleen
Living with Crohn's
You might find a food diary or app helpful when you’re speaking to your IBD team or dietitian about your diet. It can also help show whether you’re getting enough nutrients or if any foods may be triggering your symptoms. It’s important not to make any changes to your diet without speaking to your IBD team or dietitian first.
If you use a food diary or app, try to note everything you eat and drink. Include details like whether you had brown or white rice or how your food was cooked. You may find it easier to identify possible trigger foods when your condition is under control and you’re not in a flare-up.
We follow strict processes to make sure our information is based on up-to-date evidence and easy to understand.
Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishop Square, Hatfield, AL10 9NE, or contact us through our Helpline: 0300 222 5700
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
