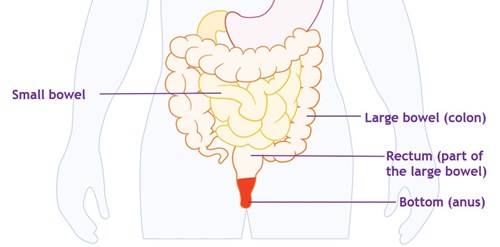
The small bowel absorbs the useful nutrients from what you have eaten. Then the liquid and non-digestible parts of food move into your colon. Usually, the colon absorbs most of the water, and the leftover waste forms a solid poo. This collects in the last part of the colon and the rectum before passing out of the body when you have a poo.
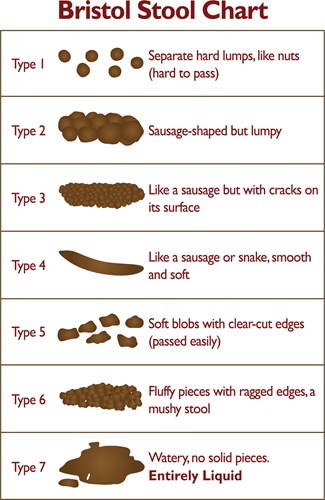
During a flare-up the cells that line the bowel become inflamed. This means that the bowel cannot absorb all the nutrients and water. This can cause watery poo, the need to poo more often and to get to the toilet quickly.
So, your diarrhoea might be due to a flare-up of your condition. But there are other factors that may be causing it or making it worse. These include:
Side effects of your Crohn’s or Colitis medicines
5-ASAs (aminosalicylates) such as mesalazine can cause diarrhoea. Some immunosuppressants, including infliximab, mercaptopurine, and methotrexate, can also cause diarrhoea. It can be hard to tell if it is your condition or your treatment causing diarrhoea. Speak to your IBD team if you’re not sure what may be causing your symptoms.
Side effects of other medicines
Diarrhoea might also be a side effect of some medicines that you may be taking for other conditions. For example, acid-lowering treatments, such as omeprazole and lansoprazole, and antibiotics can cause diarrhoea. You can check the information leaflet that comes with your medicine to see if diarrhoea is a side effect.
Colectomy and ileo-rectal anastomosis
In this surgery the colon is removed and the end of the small bowel (terminal ileum) is attached to the rectum. Because you no longer have a colon to absorb water, your poo may be quite watery. You may have to go to the toilet many times during the day and night.
Our information Surgery for Crohn’s Disease and Surgery for Ulcerative Colitis have more details about types of surgery for Crohn’s and Colitis.
Bile acid malabsorption (BAM)
Bile acids help you to digest fats. The liver makes bile acids when you eat and releases them into the small bowel. Most of the bile acids are re-absorbed in the last part of the small bowel, and returned to the liver. But, if part of your small bowel is inflamed or has been removed the bile acids are not re-absorbed. So, much higher levels of bile acids pass into the colon. This irritates the lining of the colon, which draws water into the colon causing diarrhoea.
Reduced fat absorption
If bile acid malabsorption is severe, you may not be able to digest fats from your food. So, the fats pass into your colon, causing your poo to become fatty. This is sometimes called steatorrhea. Fatty poo is greasy and runny and often smelly. It may float, so can be difficult to flush away.
Iron supplements
If you have anaemia you may have iron supplements. Iron supplements usually cause constipation. But they can cause diarrhoea in some people.
Irritable Bowel Syndrome (IBS)
People sometimes mistake IBS for Inflammatory Bowel Disease (IBD), but it is a different condition. Like Crohn's and Colitis, IBS can cause tummy pain, bloating, and loose or watery poo. But IBS does not cause inflammation of the bowel or bleeding. Some people with Crohn’s or Colitis develop IBS-like symptoms even when their Crohn's or Colitis is inactive.
Diet and food
Some people find that what they eat has little effect on their symptoms. Others find that certain foods trigger symptoms, and cutting down those foods helps. You could use a food diary or app to find out if any foods seem to affect your symptoms. It’s a good idea to discuss possible triggers with your IBD team or dietitian before making any big changes to your diet.
Changes in symptoms after eating certain foods does not always mean that your condition is flaring up. Food can sometimes trigger symptoms in people without Crohn’s or Colitis.