Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last reviewed: April 2019
Currently under review
This information is for people living with Crohn's or Colitis. It look at what may increase your risk of bowel cancer and how you can reduce this risk. It also describes changes in the bowel that may develop into cancer, and how these are detected.
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Cancer starts when cells in our body go wrong, and keep dividing and growing in an uncontrolled way. These abnormal cells can grow into surrounding tissues and organs and may spread to other parts of the body. Bowel cancer, also known as colorectal cancer, includes two types of cancer:
Bowel cancer does not include anal cancer. Anal cancer is a different type of cancer with different risk factors – around 9 in 10 cases of anal cancer are linked to human papilloma virus (HPV) infection. You can find out more about anal cancer on the Cancer Research UK website.
The symptoms of bowel cancer can be similar to those of Crohn’s and Colitis, and include:
Most people with these symptoms don’t have bowel cancer. You know your body, so if something doesn’t feel right or you are concerned speak to your doctor.
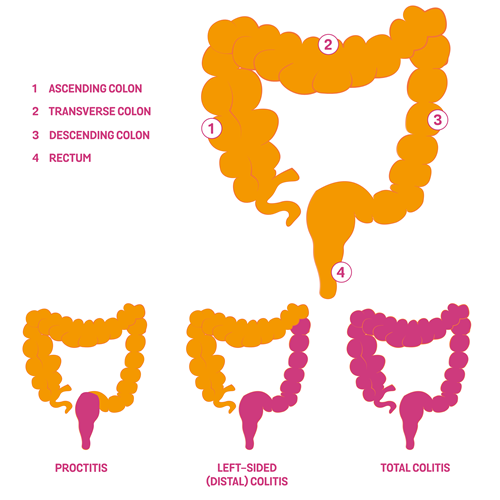
Ulcerative Colitis affects the lining of the large bowel, which includes the colon and rectum. The risk of developing bowel cancer is linked to three main factors:
The risk of developing cancer usually begins to increase about 8-10 years after the start of your Ulcerative Colitis symptoms. This is not from the date of your diagnosis, which could be much later than when your symptoms started.
Your risk of cancer is highest if all, or most, of your colon is affected by Colitis (often referred to as extensive, total or pancolitis).
If only the left side of your colon is affected by Ulcerative Colitis (distal colitis), there is less risk of developing cancer than for those with total colitis.
If your Ulcerative Colitis is limited to the rectum (proctitis), your risk is little or no greater than for the general population.
Microscopic Colitis is a condition that affects the bowel (the colon and rectum). Unlike Crohn’s Disease and Ulcerative Colitis, inflammation of the bowel lining is only visible when tissue samples are viewed through a microscope. There is no additional risk of bowel cancer in people with Microscopic Colitis.
Crohn’s can affect any part of the digestive system from the mouth to the anus. The risk of cancer in people with Crohn’s is less known.
If you have Crohn’s affecting all or much of the large colon (Crohn’s Colitis), your risk of developing bowel cancer is about the same as for someone who has had Ulcerative Colitis affecting much of their large bowel for the same length of time.
However, in a recent study, it has been found that for people with disease affecting all or much of the large bowel, about one person in every 100 might be expected to develop cancer after 10 years. This risk increases to two people after 20 years and five people after more than 20 years.
The number of people with Crohn’s or Colitis and bowel cancer has declined in recent years. This drop in numbers could be due to more widespread use of medicines for Crohn’s and Colitis which has perhaps led to fewer people having inflammation. See Are there other risk factors? below. There is better screening of Crohn’s and Colitis by colonoscopy, which might also have led to this drop. See What is a colonoscopy? But there may also be other reasons for this decline which we don’t yet fully understand.
If anyone in your family has had bowel cancer, even if they don’t have Crohn’s or Colitis, research suggests that you have an increased risk of developing cancer. The risk is greatest if you have a parent or sibling who has suffered from bowel cancer under the age of 50.
Having PSC (an inflammatory condition affecting bile ducts transporting digestive juices from the liver) increases the risk of bowel cancer. PSC is known to affect around one in 25 people with Ulcerative Colitis, and up to one in 50 people with Crohn’s. Your IBD team will tell you if you have this condition. Due to the increased risk of developing bowel cancer for people with Crohn’s or Colitis and PSC, it is recommended that people with both conditions have a yearly surveillance colonoscopy from the time of diagnosis. See Can I reduce this risk? below.
Men with Crohn’s or Colitis have been found to have a slightly higher chance of developing bowel cancer than women.
The risk of bowel cancer is higher in people over the age of 50. As there is a greater risk of bowel cancer in some people with Crohn’s or Colitis, even those under 50 should be aware of the symptoms.
Long-term inflammation is linked to developing bowel cancer, so making sure that you’re taking your medication regularly gives your bowel a chance to heal. This may mean the risk of developing bowel cancer is reduced.
Taking azathioprine or 6-mercaptopurine might protect you from bowel cancer, particularly in those who have had disease for some time and been in remission with this drug. But some studies haven’t found this effect, so more research needs to be done in this area.
If you have PSC as well as Crohn’s or Colitis, research suggests that you may be able to reduce your cancer risk by taking ursodeoxycholic acid at low doses, which is thought to work by diluting the toxic components of your bile. Your doctor or IBD team will advise you if you should take this.
Seeing your doctor at least once a year, even when your Crohn’s or Colitis is in remission, can ensure you remain on the most appropriate treatment, and that you have regular checks for any sign of cancer. Of course, if you have any
changes in symptoms at any time, it is best to speak to your doctor as soon as you can.
Regular colonoscopies (see What is a colonoscopy? below) mean that specialists can look for early changes in the colon before cancer develops. This is known as a surveillance colonoscopy. If you’ve had Crohn’s affecting the colon, or Colitis, for 8-10 years and have not recently had a colonoscopy, it’s a good idea to contact your doctor or IBD team to discuss whether this would be appropriate for you. If you have Ulcerative Colitis and PSC, you will need to have annual surveillance colonoscopies from the date of diagnosis of PSC. See How often should I have a colonoscopy? below.
If you have proctitis (inflammation of the rectum – the lower part of the large bowel) your risk is little or no greater than for the general population. You won’t need surveillance colonoscopies unless your diagnosis changes.
Physical activity and a high-fibre diet can help to prevent bowel cancer. For information on being active see our information, Living with Crohn’s or Colitis
If you have Crohn’s or Colitis and have problems with a high-fibre diet, speak to your IBD team, or ask to be referred to a dietitian.
A diet high in saturated fats and red meat may increase the risk of bowel cancer. If you eat more than 90g of red or processed meat a day, it’s recommended that you reduce your intake to 70g a day.
Red meat includes:
• beef
• lamb and mutton
• pork
• veal
• venison
• goat
Processed meat includes:
• sausages
• bacon
• ham
• deli meats such as salami
• pates
• canned meat such as corned beef
• sliced luncheon meats, including those made from chicken or turkey.
You can find more information on sizes and cutting down on red and processed meat on the NHS website.
There is more information about diet in our food section.
Alcohol has been linked to an increased chance of developing seven types of cancer, including bowel cancer. To reduce your cancer risk, it’s best not to drink alcohol at all. If you do drink alcohol, it’s recommended that you drink no more than 14 units a week and you try to spread it out over at least three days. For more guidance on drinking alcohol, see the NHS website.
Smoking is another factor which is increasing bowel cancer risk in the general population. For help and advice on how to stop smoking, see NHS SmokeFree.
We have further information on smoking and Crohn's and Colitis.
Low blood levels of vitamin D have been linked to an increased risk of colon cancer. This has been seen in people with Crohn’s and Colitis, and in the general population. More research needs to be done to really understand the link between vitamin D and colon cancer. If you have low levels of vitamin D taking a supplement may have other health benefits, such as strengthening the bones which may be weakened if you have Crohn’s or Colitis. See our information on bones. Talk to your IBD team if you have questions about taking supplements.
A colonoscopy is a type of examination that allows a specialist doctor or nurse to look directly at the lining of the colon and rectum using a colonoscope. This is a long flexible tube, about the thickness of your little finger, with a bright light
and camera at the end. It’s inserted through the anus and back passage, and it’s long enough to examine the whole colon and the end of the small intestine. The specialist can check the extent and severity of any inflammation, and whether you have any narrowed areas, polyps or dysplasia (see What is dysplasia?).
Your colon needs to be completely clean for the colonoscopy so that the specialist can get a clear view of the lining of your bowel. You’ll be asked to take a laxative either the evening before or the day of the test.
Some hospitals offer chromoendoscopy, which involves spraying special dyes onto the lining of the colon during the examination. Studies show chromoendoscopy is more effective at detecting abnormal cells lining the colon than the older technique that involved taking multiple tissue samples (‘random biopsies’) along the length of the colon. For more information on this, have a look at our tests and investigations section.
You may be offered sedation to make you feel relaxed, which many people find makes the process easier. The examination usually takes 30-40 minutes. As well as looking at the lining of the bowel, the specialist will take biopsies (small pieces of bowel lining) to examine later under a microscope in the laboratory. The specialist may also remove any polyps (small fleshy growths that form on the normally smooth lining of the colon) to examine them in more detail.
There are several different forms of polyps. The common types are:
Inflammatory polyps (including post-inflammatory polyps and pseudopolyps)
These polyps generally need no treatment, but may sometimes be removed during a colonoscopy so they can be examined under a microscope to confirm the diagnosis.
Adenomatous polyps
These polyps have the potential to develop into cancer. They are a type of dysplasia and will need to be removed (see What is dysplasia?).
Serrated polyps
These growths stick out of the surface of the colon or rectum and they are recognised by their saw-toothed appearance under a microscope. They can be difficult to find and can become cancerous. They may need to be removed.
Adenomatous polyps may be removed endoscopically (during a colonoscopy) if there is no sign of any dysplasia in the surrounding bowel wall. However, if it is not possible to remove dysplasia fully in an endoscopy, then surgery to remove all or part of the colon may be required.
It is recommended that you then have follow-on colonoscopies every 3 or 5 years or, less commonly, yearly. This will depend on what was seen during your previous colonoscopy and any other risk factors you may have. For example, you may need a colonoscopy every year if you have both PSC and Ulcerative Colitis, or have had dysplasia detected.
Having a colonoscopy is currently the best way to detect cancer early. The earlier the cancer is found, the better the survival rate. The main advantage of regular examinations is that if early warning signs are detected, treatment by endoscopy or surgery is more likely to be an option. Sometimes abnormal cells can be removed at the time of colonoscopy, avoiding the need for a surgical procedure.
Having a colonoscopy isn’t easy. Some people find the bowel preparation unpleasant. Sometimes a colonoscopy can be very uncomfortable, or it may cause bleeding or a tear of the lining of the bowel (perforation), although complications from having a colonoscopy are rare.
It is best to discuss the potential benefits and disadvantages of having regular colonoscopies with your IBD team.
In England, the NHS has recently launched a screening programme inviting all 55 year olds for a ‘one-off’ bowel scope test that looks at the lower bowel and rectum. If you’re registered with a GP and live in an area where the test is available, you’ll automatically be sent an invitation. If you are being treated for your Crohn’s or Colitis, you may not be able to have this test. You can contact the NHS free bowel cancer screening helpline for further information. See Other organisations for details.
The NHS has a bowel cancer screening programme for those between 60-74, using a Faecal Occult Blood (FOB) test. This test, which is sent through the post every two years, does not diagnose cancer, but looks for hidden blood in your bowel motions (stools), which could be due to cancer.
If blood shows up in your stool in the FOB test, this may be due to your Crohn’s or Colitis, rather than another condition. Blood in your stool can mean that there is inflammation in your bowel, even if you don’t have any symptoms of diarrhoea or bleeding. If the inflammation is confirmed in a colonoscopy, treatment can be prescribed to heal the bowel.
If you receive an invite for the FOB test, it is worth telling them that you have Crohn’s or Colitis and when your last colonoscopy was. They will be able to discuss whether the screening is necessary for you. You could also let your IBD team know that you have received an invite for bowel screening and they will be able to advise you further.
Other methods for detecting bowel cancer are being researched. For the time being taking your medication regularly, maybe adjusting your diet and, if appropriate, having regular colonoscopies, are likely to be the most effective ways of reducing your risk of bowel cancer.
If you are diagnosed with bowel cancer, your healthcare team will discuss the benefits and risks of the different treatment options available. One of those options may be surgery, and possibly a stoma. See our Living with a Stoma information for more details about this procedure.
If you would like more information on bowel cancer, diagnosis and treatment, see the websites for Bowel Cancer UK and Cancer Research UK. They offer additional services such as an email enquiry service to nurses, and a helpline,
which might be helpful if you have questions. See Other organisations for further details.
020 7940 1760
Email: nurse@bowelcanceruk.org.uk
Scotland: 0131 281 7351
Email: scotadmin@bowelcanceruk.org.uk
Cancer Research UK
Helpline: 0808 800 4040
Macmillan Cancer Support
020 7840 7840
Helpline: 0808 808 00 00
NHS Bowel Cancer Screening Programme
England: 0800 707 60 60
Scotland: 0800 0121 833
Wales: 0800 294 3370
Northern Ireland: 0800 015 2514
Health professionals can order some publications in bulk by using our online ordering system. If you would like a printed copy of any of our information, please contact our helpline.
Our helpline is a confidential service providing information and support to anyone affected by Crohn's or Colitis. Our team can:
Email helpline@crohnsandcolitis.org.uk
This closed-group community on Facebook is for everyone affected by Crohn's or Colitis. You can share your experiences and receive support from others.
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn's or Colitis. All events are open to members of Crohn’s & Colitis UK.
We follow strict processes to make sure our information is based on up-to-date evidence and easy to understand.
Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishop Square, Hatfield, AL10 9NE, or contact us through our Helpline: 0300 222 5700
Living with Crohn's or Colitis
Read information
Healthcare
Read information
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Signposting you to specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
