Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last updated: April 2025
Last full review: October 2024
Next review date: October 2027
You may not have heard of Ulcerative Colitis before, or Colitis as we’ll refer to it. It’s a type of Inflammatory Bowel Disease, or IBD, which we’ll explain more about later. In Colitis, parts of the large bowel become swollen, inflamed and ulcerated. This can cause diarrhoea, blood in your poo, weight loss, tiredness and tummy pain, and you may have other symptoms too.
Being told you have Colitis can be a shock. You might feel anxious or unsure about what comes next and how your life might change. But you’re not alone.
Now that you’ve put a name to your symptoms, you can start to manage them. And we’re here to help, every step of the way.
This information is for anyone who has Colitis, thinks they might have it or wants to learn more about it. It looks at:
This information might use words you have not heard before. Our page on medical words can help provide an explanation.

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Ulcerative Colitis is an Inflammatory Bowel Disease, or IBD, which causes problems with your immune system., This causes swelling and inflammation in your rectum and colon, which are two parts of the large bowel. Colitis can be diagnosed at any age, most people are diagnosed between the ages of 20 and 40 years. At least 1 in every 233 people in the UK live with Ulcerative Colitis.
Other forms of IBD include Crohn’s Disease and Microscopic Colitis. It may not always be possible for doctors to tell the difference between Colitis and Crohn’s Disease if the inflammation only affects your colon. In this case, you may be diagnosed with IBD Unclassified, also known as IBD-U or Indeterminate Colitis.
You may have been diagnosed with Crohn’s Colitis, which is a type of Crohn’s. It doesn’t mean you have both Crohn’s and Ulcerative Colitis. Find out more in our information on Crohn’s Disease.
As many as 1 in 10 people with Ulcerative Colitis will have their diagnosis changed to Crohn’s or IBD-U in the first five years.
We refer to Ulcerative Colitis as ‘Colitis’ in this information. The term ‘colitis’ by itself is a general term that means inflammation in the colon. There are different types of colitis. Some are not types of Inflammatory Bowel Diseases and are different to Ulcerative Colitis. These include:
IBD is not the same as IBS, which stands for irritable bowel syndrome. IBS has some symptoms that are similar to Colitis. But this is a different condition and treatment for IBS is not the same.
Colitis is not contagious; you can’t catch it. There's nothing you could have done differently that would have stopped you from developing Colitis.
Colitis is a lifelong condition and can be hard to predict. Sometimes you may feel well and have no or few symptoms, known as remission. At other times symptoms may be more active or difficult to manage, known as flare-ups or relapses.
Right now, there is no cure for Colitis. But there are many effective treatments to help you control symptoms and prevent long-term problems. Treatment options may include medicines, surgery, and sometimes a combination of both. Working together, you and your healthcare professionals can find a way to manage the condition that works best for you.
I try and take each day as it comes. I have learnt that I need to take it easy sometimes, but it hasn’t stopped me doing the things I enjoy. I like running, so I get out for a run when I feel up to it.
Andy
Living with Colitis
Coming to terms with having Colitis can take time. It’s common to go through a period of adjustment as you get used to everything, learn more about the condition and find your own ways of living well.
Everyone is different – there’s no right or wrong way of doing things. You may feel more in control if you learn all you can about your condition, or you may find that taking things one step at a time is better for you. If you are finding things difficult, our information on mental health and wellbeing can help you find out how to get the help you need.
Life is difficult with Ulcerative Colitis with so many flare-ups and medicines, but I am keeping up with it.
Ahad
Living with Colitis
Have you recently been diagnosed with Crohn’s Disease, Ulcerative Colitis or Microscopic Colitis?
Our eight, bite-sized, weekly emails can help you:
Sign up to our new series of emails to help you navigate life after diagnosis.
Everyone with a diagnosis of Colitis should be seen by an IBD specialist and cared for by a team of healthcare professionals. This team will be led by a consultant gastroenterologist. This is a doctor who specialises in the digestive system. All teams are different but are likely to include IBD nurse specialists and surgeons. Some IBD teams may include a gastroenterology dietitian, expert pharmacist and psychologist. They will refer you to any other health professionals you might need to see.
Your specialist team should be able to support you with every aspect of your care. This includes your first assessment and diagnosis, treatment, and rapid care during flare-ups. They can offer nutritional help and support you through surgery if you need this. But remember, although they are experts in Colitis, you will become the expert in how the condition affects you.
I have a good relationship with my local hospital and am fortunate to have an excellent IBD nurse. Knowing that I can contact her when I start to experience a flare-up, and knowing that she will help as much as she can, helps to reduce the stress of the situation and speed up treatment.
Andrew
Living with Colitis
Our appointment guide will help you get the most out of your appointments. It can help you understand what matters most to you about your treatment and care.
The gut is the part of your body that takes food and nutrients in and carries poo out. The gut starts at your mouth, when you eat, and ends at your bottom, or anus, where poo passes out of your body.

The bowel is the largest part of the gut and is made up of two sections. These are the small bowel and the large bowel. The large bowel starts at the beginning of the colon and ends at the anus. It includes the colon and rectum. Colitis usually begins in the rectum and lower colon, but it may involve all of the large bowel. If your rectum is the only part that’s inflamed, it’s called proctitis.
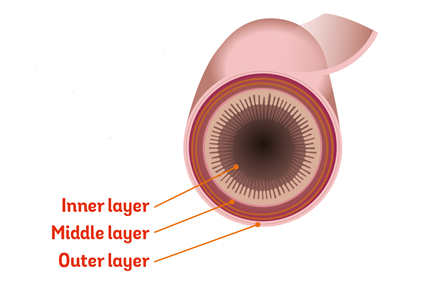
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, there’s inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. Ulcers develop on the inner layer as the condition gets worse, but they can also heal as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When you’re having symptoms, it’s known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section types of Colitis.
The most common symptoms are:
Colitis is a bowel condition, but having an overactive immune system and ongoing inflammation can sometimes lead to problems in other parts of the body. Some people experience inflammation in their joints, eyes, or skin. See the section on complications outside the bowel.
A flare-up is when symptoms come back, and you feel unwell. Everyone experiences flare-ups differently. Your symptoms may also change over time. Flare-ups can last anywhere from a few days to several months and you may have different symptoms during a flare-up than you had when you were first diagnosed.
Flare-ups may not happen very often – people can go years without feeling unwell. For others, flares may happen more often, with two or more a year.
Over time you’ll get to know how to recognise a potential flare-up. Working together with your health professionals, you’ll create a treatment plan for flare-ups. The plan will give guidance on what to do and who to contact. This may be your IBD team, their advice line or your GP.
Signs of flare-up can include:
If you’re worried in any way, contact your IBD team or your GP. Fast access to the healthcare team who know you will provide the support and reassurance you need.
A flare-up can also affect other parts of the body and cause:
In some cases, your IBD team or GP may use blood tests, poo tests or endoscopy to check if you’re having a flare-up. The results will help to find the best treatment to control your Colitis. See the sections on tests and treatments.
Flare-ups can be disruptive. Sometimes you may need to cancel plans or take time off work when you feel unwell. It can help to be open about your condition with your family, friends, work colleagues and employers. Our talking toolkit can help.
It is important to know the difference between your 5-ASA dosage for maintaining remission, and your dosage for managing a flare-up. This has given me opportunities for early intervention when I feel like I am about to become unwell.
Andy
Living with Colitis
Taking your medicines as prescribed by your IBD team, even when you feel well, reduces the risk of flare-ups. We don’t yet know what causes flare-ups, but possible triggers include:
It can help to keep a diary of symptoms to help you spot any triggers. You can find one in our appointment guide
Colitis happens when the body’s immune system goes wrong. Usually, the immune system protects the body against harmful substances and infections. It is thought that in Colitis, the immune system starts attacking the bowel. When it comes to understanding what causes Colitis, there's still a lot we don't know.
We don't know for certain if Colitis is an autoimmune condition, but some experts think it might be. This is because in Colitis, the immune system seems to attack the bowel, which is something that happens in autoimmune conditions. We haven't found a clear reason or trigger for why this happens in Colitis. Researchers believe that a mix of genes, bacteria in the gut and the environment probably cause Colitis, but more research is needed to know for certain.
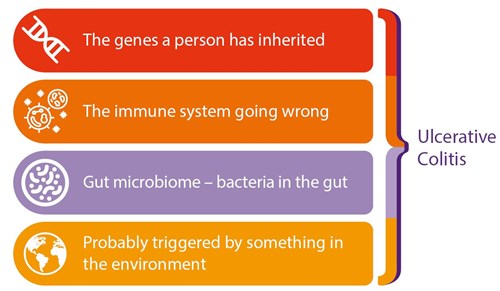
Researchers have identified hundreds of genetic changes that affect your risk of developing Colitis. Many of these changes are in genes that control the immune system. Changes in these genes may alter the immune system's response to bacteria in the gut. This can lead to ongoing inflammation.
Some genes associated with developing Crohn’s or Colitis might be specific to certain ethnicities. A lot of studies on Crohn’s and Colitis do not collect data on ethnicity. This makes it difficult to understand how ethnicity affects Crohn’s or Colitis.
In Colitis, something goes wrong with the immune system. Research suggests that in Colitis the protective gut barrier is faulty. The gut barrier allows important nutrients into the gut and keeps harmful substances out. Without this layer of protection, the immune system starts attacking certain bacteria or viruses that live in the gut. This causes inflammation.
The gut microbiome, sometimes called the gut microbiota or gut flora, is the natural bacteria, viruses and fungi that live in your gut. It is thought that in people with Colitis, there may be an imbalance of good and bad bacteria in the bowel.
A range of factors in the environment may increase the risk of Colitis. These include:
Colitis is more common in non-smokers and for some people, stopping smoking may trigger Colitis. Smoking carries many other health risks. See our information on smoking. There’s still no definite evidence that any one of these factors is the cause of Colitis.
The types of Colitis are based on how much of your large bowel is affected. This can affect the symptoms you experience and the treatment you’re offered. You may not know which type of Colitis you have when you are diagnosed. This may depend on whether you have had:
See the section on tests and treatments.
The main types of Ulcerative Colitis are:
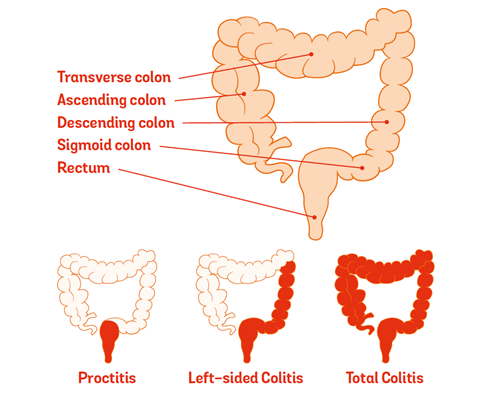
In proctitis, only the rectum, or the lowest part of the large bowel, is inflamed. The rest of the colon is unaffected and can still function normally.
Common symptoms may include:
1 in 10 people with proctitis will later develop Colitis that affects most of their colon.
Proctosigmoiditis affects the rectum and the part of the colon next to the rectum, called the sigmoid colon.
Common symptoms may include:
For this type of Colitis, inflammation is found in the distal colon. This includes the rectum and the left side of the colon, which is also called the descending colon.
Common symptoms may include:
Colitis that affects the whole colon is known as total Colitis or pancolitis. If the inflammation affects most of the colon, but not all, it is known as extensive Colitis.
Common symptoms may include:
In milder flare-ups, the main symptom may be diarrhoea or looser poo without blood.
For some people with total or extensive Colitis, inflammation may reduce over time, so their Colitis may affect less of the colon.
When you have symptoms, your condition may be described as being ‘active’. If your Colitis is very active it may mean you are having a flare-up.
Colitis is different for everyone. Your IBD team will assess how severe your Colitis is to help find the best treatment for you. This will be based on your symptoms, how Colitis impacts your daily life and your test results.
The following severity groups are only a guide. It is common to be between two severity groups. For example, your IBD team may say you have mild-to-moderate Colitis or moderate-to-severe Colitis.
ASUC is a serious medical emergency that requires a stay in hospital for treatment and monitoring. Symptoms include all those for ‘severe’ Colitis, as well as signs that the body is being significantly affected by the disease such as a fever or increased heart rate.
In very rare cases, Colitis can cause other problems in the bowel. These complications include:
When inflammation is extensive and severe, the bowel wall thins and the colon becomes bloated with gas. This is known as toxic megacolon. Symptoms include a high fever with pain and tenderness in the tummy. It’s essential to get treatment quickly. There is a large risk of perforation, see below. You may also be at risk of developing sepsis. Sepsis is a life-threatening over-reaction of your immune system to an infection. Emergency surgery may be needed.
A perforation is a rupture of the bowel. This creates a hole that contents of the bowel may leak through. They can be caused by:
Perforations are very rare, but very serious. Symptoms can include:
Contact NHS 111 straight away if you think you have signs of a perforation or toxic megacolon.
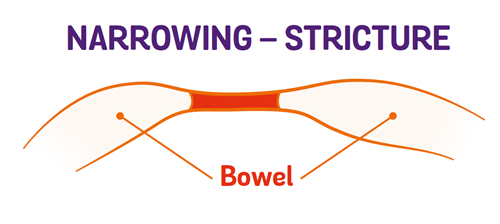
Ongoing inflammation can create a narrow section of the bowel known as a stricture. A stricture can make it difficult for poo to pass through. If it’s very narrow it can cause a blockage.
Strictures are rare in Colitis, but they can sometimes be a sign of bowel cancer. For more information, see the section on Risk of cancer. Even though most strictures are not cancer, known as benign, they may still need surgery.Colitis doesn’t just affect the bowel. As many as 1 in every 5 people with Colitis develop problems in other parts of the body. The most affected parts of the body are the joints, eyes or skin. These are known as extraintestinal manifestations, or EIMs. They usually happen during a flare-up but can occur without or before any bowel symptoms.
For many of the complications, there are things you can do to reduce your risk.
You may have pain with or without swelling in your joints. Around 1 in 5 people with Colitis experience joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in our information on joints.
Eye problems are also common for people with Colitis.
Episcleritis affects the layer of tissue covering the white outer coating of the eye, the sclera, making it:
This tends to flare up at the same time as bowel symptoms. It often gets better with treatment for Colitis or with steroid eye drops.
Uveitis is inflammation of the iris and scleritis is inflammation of the sclera. These are serious and can lead to loss of vision if they’re not treated. Symptoms include:
They’re treated with steroid drops, and sometimes immunosuppressants or biologic medicines.
These are not to be confused with conjunctivitis, which is a common eye condition that is not associated with Colitis. Conjunctivitis causes redness and irritation and produces sticky pus.
If you get any kind of painful eye irritation, redness or inflammation, tell your healthcare professional. They may refer you to an eye specialist.
Colitis can affect the skin in different parts of the body.
Erythema nodosum affects between 2 and 10 in every 100 people with Colitis. It causes raised, painful patches of skin that look red or darker than the surrounding skin. It is often found on the legs. It usually occurs during flare-ups and usually improves with treatment for Colitis.
Pyoderma gangrenosum is a less common condition in people with Colitis. This starts as small tender blisters or pustules, which become painful, deep ulcers. On brown or black skin, the skin around the edge of the ulcer might be darker. Pyoderma gangrenosum can occur anywhere on the skin, but most commonly appear on the legs, or near stomas. This condition is sometimes, but not always, linked to a flare-up. It’s often treated with steroids or biologic medicines, such as infliximab. In some cases, a specialist in skin conditions, known as a dermatologist may treat this with creams or ointments.
Around 1 in 5 people with Colitis develop anaemia. There are several types of anaemia. People with Colitis are likely to develop iron deficiency anaemia. It is caused by a lack of iron in your diet, poor absorption of iron from food, or blood loss from the gut. Your body needs iron to help make red blood cells, which carry oxygen around your body.
Anaemia can make you feel very tired. If it’s more severe you may also have:
Treatment depends on the cause of anaemia. You may be prescribed iron supplements that are taken by mouth. Or you may be given iron into your vein, known as intravenously, either by an injection or infusion through a drip. Find out more about iron in our information on other treatments.
People with Colitis are more at risk of developing thinner and weaker bones, known as osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for making bones, and this may be low if your diet doesn’t contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. For some people, medicines can be helpful. Find out more in our information on bones.
Primary Sclerosing Cholangitis, known as PSC affects around 1 in every 100 people with Colitis. PSC causes inflammation of the bile ducts and can eventually damage the liver. Symptoms can include:
Some people do not get any symptoms and it may only be picked up on blood tests.
Some medicines used to treat Colitis, such as azathioprine, can affect the liver. Changing your treatment may help to reduce this type of liver complication.
It is also common for people with Colitis to get sores or ulcers in their mouth, usually when their condition is active. These sores can be minor and disappear within a few weeks but can occasionally last longer and may need topical steroid treatment.
Losing more hair than usual is common with Colitis. Many things can trigger this, including severe flares, poor nutrition, iron and zinc deficiency and surgery. This type of hair loss is called telogen effluvium. Less often, hair loss may be a side effect of medicines. You should not stop taking a medicine unless your doctor has told you to. Losing your hair can be distressing, but it’ll usually grow back as you get better. Speak to your IBD team to check what might be causing your hair loss.
People with active Colitis may have a slightly increased risk of cardiovascular disease, including heart problems and strokes.
You can reduce the risk of having heart problems or a stroke by:
Call 999 immediately if you think you may be having a stroke or heart problem.
You’re more likely to develop blood clots if you have Colitis. This includes deep vein thrombosis, known as DVT, in the legs, and pulmonary embolisms in the lungs.
You’re more at risk:
To reduce your risk:
These precautions can also be helpful when you travel by plane, car or train for more than three hours, which increases the risk of blood clots for everyone. Find out more in travel.
If you’re staying in hospital because you’re unwell with your Colitis, you may be offered a medicine or injections to prevent blood clots.
Although some symptoms are similar, IBS is a different condition to IBD. IBS can cause tummy pain or cramps, but these are often worse after eating and better after a poo. IBS can also cause bloating, diarrhoea and constipation. IBS is more common than IBD. Colitis causes inflammation in the bowel and blood in poo, but IBS does not.
Some people with Colitis also develop IBS symptoms and they may have pain and diarrhoea even when Colitis isn’t active. Doctors can use a poo test called faecal calprotectin to check if you’re having a Colitis flare, which causes inflammation, or if your symptoms could be IBS. IBS treatment can include changes to diet and lifestyle and medicines to ease symptoms.
Bowel cancer usually affects the large bowel. It is also known as colorectal cancer, or CRC.
If you have Colitis, you are more likely to develop bowel cancer than the general population. But the actual increase in the risk of developing bowel cancer if you have Colitis is low. And over the last 20 years, the number of people with Colitis who develop bowel cancer has fallen.
The risk of bowel cancer increases from around eight to ten years after the start of your Colitis symptoms. This may not be when you were diagnosed, as your symptoms could have started sometime before diagnosis.
If you have Colitis, the risk of developing bowel cancer is linked to how much of your large bowel is affected:
Primary Sclerosing Cholangitis, or PSC, is a condition that affects some people with Colitis. Having PSC also increases your risk of bowel cancer. Find out more about PSC in the section complications outside the bowel.
If you are at increased risk of bowel cancer you will be offered regular colonoscopies to check for early warning signs. Cancers can be more successfully treated when found early. Long-term inflammation is linked to developing bowel cancer. Following your treatment plan and taking your medicine as prescribed gives your bowel a chance to heal. This may reduce your risk of developing bowel cancer.
People with Colitis are at higher risk of bile duct cancer compared with the general population. Your bile ducts are tubes that connect your gallbladder and liver to your small bowel. Having primary sclerosing cholangitis, known as PSC, is also a risk factor for developing bile duct cancer. So, if you have PSC and Colitis, your risk of developing bile duct cancer may be even higher.
In very rare circumstances, some medicines for Colitis can increase the risk of other cancers. The risk is very small and the benefits of taking the medicines will most often outweigh the possible unwanted effects. Check the leaflet that comes with your medicine for precautions you can take to reduce this risk. Talk to your IBD team if you would like to find out more.
Find out more in our information on the risk of bowel cancer and other gut-related cancers.
People who have Colitis can generally expect to live a long life. Some researchers have found that people with Colitis live just as long as people without Colitis. Others have found that people with Colitis might have a slightly shorter life expectancy. Many other factors can also affect life expectancy, so it’s hard to know what is linked to Colitis and what is not.
Research on life expectancy usually looks back at what has happened to people with Crohn’s or Colitis over several decades. Treatment options were much more limited in the past. So we do not know if the data that’s available reflects what is happening today, with all the new treatments we now have. We do know that life expectancy is increasing for people with Crohn’s or Colitis.
To find out if you have Colitis, you may have had lots of tests. The same tests help your doctors check your health and find the best treatment for you. Your Colitis should be checked regularly. How often you need these tests will depend on how severe your Colitis is, and the medicines you are taking. Tests for Colitis include:
Doctors will ask you about the gut symptoms you have been having, how often you have them, and how much they affect you. You may also be asked about symptoms involving other parts of your body, such as your skin, eyes and joints.
Your doctor may also ask you about:
Your IBD team can examine the outside of your body. They may ask about or check:
Blood tests can show whether you have inflammation somewhere in your body and if you have low iron, known as anaemia. They can also check whether the medicine you take for your Colitis is causing any side effects.
Poo tests are also used to see whether you have an infection. Your poo can also be tested for signs of inflammation. A faecal calprotectin test can show whether you have inflammation in your bowel.
A doctor will look at the lining of your gut with a tiny camera on a long thin flexible tube. This is called an endoscope. Endoscopy is the best way to look at the large bowel. It helps your doctor see if your Colitis is well-controlled, or if you still have inflammation.
The doctor may take very small samples of bowel tissue during an endoscopy. These are called biopsies. There is usually no pain when biopsies are taken. These are sent to the laboratory and examined under a microscope to check for inflammation.
Other tests that look at where inflammation is in your gut include MRI, also called a Magnetic Resonance Imaging, and CT scan, known as a Computerised Tomography scan. MRI and CT are usually used to look at the small bowel to rule out Crohn’s but can also be used to check for complications of Colitis.
You may need a few of the tests listed above. You can find out more in our information on tests and investigations. Your IBD team should provide you with information about timescales and a point of contact in the IBD team while you’re waiting for the results of any tests.
Everyone with a diagnosis of Colitis should see an adult or paediatric gastroenterologist, depending on your age. They will often be part of a team that could include:
Find out more in the section on your IBD team.
The IBD Standards set out what ideal care should look like. But every hospital is different, and your team or care may vary.
You should be able to start treatment within 48 hours of being diagnosed with Colitis if you have moderate to severe symptoms. If your symptoms are mild, you should be able to start treatment within two weeks. However, based on the experiences shared with us, we understand this is not always the case and there may be long waits to start treatment. We are working hard to ensure everyone with Colitis has access to the right care, support and treatments at the right time. Find out more about what we are doing to improve your healthcare.
Treatment aims to stop the inflammation so your bowel can heal, and your symptoms reduce so that you enter remission. This will help you to feel better. It can also reduce the risk of complications or your Colitis getting worse. Treatment is often needed long-term to help keep you in remission.
Treatment for Colitis may be with medicines, surgery, or a combination of both.
You should work with your IBD team to decide on a treatment together. Your treatment will depend on how Colitis affects you. This will include:
It’s important to think about what matters most to you about your treatment and care. This will help you and your IBD team find the treatment that’s right for you. Find out more in our appointment guide. Your IBD team should help you understand all the treatment options available and their benefits and risks.
If your condition is mild and your gut looks healthy, you may consider stopping treatment. You should first discuss the risks and benefits of this with your IBD team.
Medicines can be very effective in treating your symptoms. They can help to prevent your condition from getting worse or causing complications.
Medicines sometimes cause side effects, but your IBD team will monitor these carefully. Medicines do not work the same way for everyone. It is not always possible for your IBD team to predict which treatment will suit you best. It is important to make sure you find a medicine that works for you. It may take some time to find the right medicine for you.
Use this tool to understand more about potential treatment options that suit your needs. The tool is designed to help you:
You may take one medicine or a combination of medicines. The main types of medicines are:
Other names: balasazide, mesalazine, olsalazine, sulfasalazine.
5-ASAs reduce inflammation in the lining of the bowel and help to keep you in remission. 5-ASAs are often the first treatment option for mild to moderate Colitis. See our information on 5-ASAs.
Other names: beclometasone dipropionate, budesonide, prednisolone.
When you’re in a flare-up, steroids can quickly reduce the inflammation in your gut to help you feel better. Some types of steroids have a higher risk of side effects. Steroids cannot be used to control Colitis long-term. You’ll only take steroids for a set amount of time. Your doctor may then suggest a different medicine that can help to keep you well and in remission. Find out more in our information on steroids.
Other names: azathioprine, mercaptopurine.
These dampen down the immune response, which reduces inflammation in the gut and helps to prevent flare-ups and reduce symptoms. They may help you reduce or stop taking steroids without having another flare-up. They may also help if the inflammation hasn’t been controlled by 5-ASAs. See our information on azathioprine and mercaptopurine.
Biologic names: adalimumab, golimumab, infliximab, mirikizumab, risankizumab, ustekinumab, vedolizumab.
Other targeted medicine names: etrasimod, filgotinib, ozanimod, tofacitinib, upadacitinib
Biologics and other targeted medicines are treatments that block particular proteins or chemical pathways involved in inflammation. This reduces inflammation and helps get your Colitis under control and keep it under control. They also alter your immune system, so you might not fight off infections as well as other people.
Find out more in biologic and other targeted medicines and in our individual medicine information.
You can live a full and happy life with Ulcerative Colitis – it hasn’t stopped me doing anything! Medicines have kept me well for most of the 30+ years since my diagnosis.
Paul
Living with Ulcerative Colitis
The medicines you take will depend on how severe your Colitis is.
| Colitis Severity | Possible treatment options |
|---|---|
|
Mild to moderate Colitis
|
You may first be offered 5-ASAs. Your doctor may suggest a certain type, depending on where the inflammation is in your bowel. The 5-ASA you are offered may be topical, such as enemas or suppositories that are inserted in your bottom, or oral, including tablets, capsules or granules that you take by mouth. 5-ASAs may be taken long-term to keep your condition under control. If 5-ASAs don’t work or are not right for you, you may be offered topical steroids. Some people will also take an oral steroid, such as prednisolone. Other people may be offered oral steroids that work specifically in the bowel, such as Budesonide MMX or beclomethasone dipropionate. Steroids can’t be taken long-term, so you may be offered azathioprine or mercaptopurine to keep your Colitis under control. |
| Moderate to severe Colitis |
You may first be offered oral steroids, such as prednisolone. If you’re very unwell you may be given steroids by an infusion in hospital. Steroids can’t be taken long-term, so you may be offered azathioprine or mercaptopurine to keep your condition under control. Some people may be offered 5-ASAs instead. If these medicines don’t work or aren’t right for you, you may be offered a biologic or other targeted medicine. You can take these medicines long-term to keep your condition under control. Some people may take azathioprine or mercaptopurine in combination with their biologic medicine. |
|
Acute Severe Ulcerative |
You’ll stay in hospital and may be treated with a high dose of steroids given through a drip into a vein in your arm. This is known as an infusion. After three days, if steroids haven’t worked you may be given infliximab or ciclosporin. After seven days, if infliximab or ciclosporin have not worked surgery may be necessary. |
Some medicines can help to ease symptoms, but don’t reduce inflammation or treat the underlying Colitis.
Talk to your doctor or IBD team before you take these or other medicines you can buy yourself. They may make your symptoms worse, can cause blockages or could interact with other medicines you’re taking.
Find out more about these medicines in our information on other treatments.
If medicines aren’t helping and flare-ups keep happening, then surgery may be an option. Many people think surgery is the last option, but that isn’t true. Surgery is offered when doctors think it will help your symptoms.
Most people with Colitis will have planned surgery, so you’ll have time to discuss all of your options and prepare. You’ll see a surgeon who will explain what will happen and give you the chance to ask any questions you have.
More rarely, people with very severe Colitis or severe complications may need urgent surgery within a few days or emergency surgery within a few hours.
You may be offered surgery if:
Recent studies show that:
The most common operations for Colitis removes part or all of the large bowel. Find out more, including videos and diagrams, in our information on surgery for Colitis.
If you have a large part of the bowel removed, you may need a stoma. A stoma is an opening through the tummy, made during surgery. The end of the bowel is brought outside the body through this opening, onto the surface of the tummy. Poo then passes out of this opening, and into a disposable bag that is worn over the stoma.
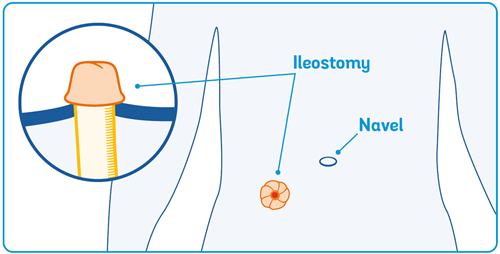
Both types of opening are called a stoma, and the bag is known as a stoma bag. A stoma may be temporary or permanent.
Having a major part of the bowel removed may be a frightening thought. You may also be concerned about using a stoma bag. However, there have been big improvements in the design of stoma products. They are now very discreet and comfortable.
A stoma nurse will support you and give you practical help and information on living with a stoma.
You can find out more in our information on living with a stoma. There are lots of personal experiences of people living with a stoma on our website and Facebook Forum. There are also other organisations that can give practical advice and support – see their contact details at the end of this guide.
I am amazed how many people are surprised to hear I have a bag. Obviously, it’s not ‘obvious’!
Annie
Living with Colitis
Colitis isn’t a visible illness so it’s important to find your own way of describing the nature of your condition. Other people will not know what we need from them unless we tell them!
Rose
Living with Colitis
When you live with Colitis it can help to have the understanding and support of those around you. But it takes guts to start the conversation.
Our talking toolkit can help. From opening up about mental health, speaking with your boss or talking to children, there are lots of important conversations you may need to have. Talking about your Colitis will help people understand what it’s like to live with Colitis, how it affects you and how they can help.
We have information for friends, family and employers. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohn's and Colitis together. They are run by volunteers and host a range of events, from educational talks to social events. We also offer virtual social events. The events are a chance to chat and share experiences with others across the UK. Check our website or call our helpline to find your nearest Local Network or the next virtual social event.
Be open about your condition with friends, family, colleagues and even sports coaches. Everyone I’ve told has been nothing but understanding, accommodating and supportive – and I feel great knowing people are there for me.
Kate
Living with Colitis
Having Colitis and its treatments can also have emotional effects on your personal and sexual relationships. Your body image may change, you may feel embarrassed by some of your symptoms or you may not feel up to having sex. This can have an impact on your relationship, or you may feel discouraged from starting a new relationship. Our information on sex and relationships includes some suggestions that might help you deal with any difficulties, and shares other sources of help and advice.
There isn’t any clear evidence that specific foods cause, cure or treat the inflammation in Colitis. It’s important to try to eat a healthy, balanced diet that gives you all the nutrients you need to stay well.
When you’re feeling unwell, it can be difficult to eat enough of the right nutrients to stay well and keep a healthy weight. You might not feel like eating much, or you might only be able to tolerate certain foods. You may have a low appetite or lose weight without trying to. Some people might gain weight. This could be because of changes to your diet, or as a result of some treatments for Colitis, such as steroids.
Some people find that what they eat has little effect on their symptoms. Others find that certain foods trigger symptoms and cutting down on those foods helps. There is no particular diet that works for everyone with Colitis. What works for one person might not work for another.
It’s important to get advice from your IBD team or dietitian before you make any major changes to your diet. A food diary can be a handy tool to help you when you speak to your health professional about your diet. It may help to show whether you’re getting enough nutrients or if any foods may be triggering symptoms. You can find one in the information on food and in our appointment guide.
Your healthcare professional may recommend a liquid food supplement. This can help make sure you’re getting all the energy and nutrients you need.
I have to be careful now that I have an ileostomy, as certain foods don’t digest well, and can cause blockages, which are not only painful, but can be very dangerous.
Katryna
Living with Colitis
You may need to take supplements to replace low levels of vitamins and minerals. This can happen when you have a poor appetite, do not eat enough, or when you have ongoing diarrhoea. Your doctor, dietitian or IBD nurse will tell you if this is the case. The most common vitamin and mineral deficiencies are:
Around 1 in 3 people with Colitis have low iron levels. This could be because you’re not getting enough iron in your diet, you’re losing blood, or you have problems absorbing iron from food. Low iron levels can lead to anaemia, where you do not have as many red blood cells as you should to carry oxygen around your body. This can make you feel tired, breathless or dizzy.
If you have low iron, you may be given iron supplements as tablets by mouth, by injection or as a drip, known as an infusion, into a vein.
Calcium and vitamin D help keep your bones and teeth healthy. But many people with Colitis have low levels.
If your Colitis is active, or you’re taking steroids, you should have a blood test to check your vitamin D levels. Blood tests are not helpful to check for low calcium levels, but your IBD team might check how much calcium you get in your diet instead.
You may need to take supplements if your calcium or vitamin D levels are low. Getting enough calcium and vitamin D is especially important for people who are going through menopause or have already gone through it.
Many people with Colitis try complementary or alternative therapies to help manage their condition.
There is some limited evidence that some of these therapies may help manage Colitis symptoms. But there is not enough to recommend them as treatments. These include:
Other therapies include homeopathy, herbal medicines, acupuncture and other traditional Chinese medicines. There has been little or no evidence that these types of therapies work.
If you decide to try any of these approaches you may want to consider:
Find out what qualifications your complementary therapist has. Many complementary therapists aren’t regulated as other health professionals are.
Don’t forget to talk to your doctor first, especially if you’re thinking of taking any herbal medicines. There may be interactions with some prescription medicines.
Find out more about complementary and alternative therapies in our food and other treatments information.
Taking care of your mental health is just as important as taking care of your physical health. Mental health is a major part of living with Colitis. Research suggests that people living with Crohn’s or Colitis may be twice as likely to experience mental health problems, like anxiety and depression, as the general population. And around half of all people with Crohn’s or Colitis say it has affected their mental health in some way.
You are more likely to experience poorer mental health at certain times such as:
It can help to be aware of the times when you may be at greater risk of changes in your mental health. You can then get the help and support you need.
There are lots of positive things you can do for yourself to influence the course of your Colitis – but acknowledge that you do not need to deal with this alone.
Ros
Living with Colitis
Living with a long-term condition like Colitis can trigger lots of different feelings and emotions. You might feel shocked or a sense of disbelief when you are first diagnosed, and find it hard to adjust. You may feel anxious, frustrated, sad, scared, or angry about having the condition and dealing with distressing symptoms. Not knowing what might happen in the future may make you feel helpless and uncertain. You may feel very isolated or even ashamed about your condition.
These feelings are completely normal, and many people with Colitis experience them from time to time. It’s not a sign of weakness. Long-term health conditions are a lot to deal with, and it’s natural that you might struggle to cope sometimes. Give yourself time and space to accept your feelings. For some people, these negative feelings can become overwhelming. This can lead to mental health problems like stress, anxiety, and depression.
It can be helpful to understand more about your mental health, recognise the feelings and know what you can do. Getting support in place and developing coping strategies can help. You’re not alone. We’re here to help.
Being in the present moment is my key… you can’t change the past or control your future. Being in the present moment and taking it day by day really helps me to reduce anxiety.
Sharon
Living with Colitis
A mood diary or mood tracker app can help you keep a record of how you’re feeling. You can also share this with your IBD team. Our mental health and wellbeing resource has information on things you can do to improve your mental health and get the help you need.
We understand that it is not always easy to be physically active if you’re living with Colitis. But being active is important for physical and mental health. It is safe to be physically active or to exercise with Colitis. Current research suggests it does not cause flare-ups.
You might find it difficult to be active if your Colitis is severe. Symptoms like tummy or joint pain, fatigue, or urgently needing to poo can get in the way. Most people with Colitis say exercising makes them feel better. Some said they have more energy, sleep better and have fewer gut symptoms.
If you’re not very active or your symptoms are making it difficult, try to build up your activity levels slowly. Walk to the shops instead of taking the car, use the stairs instead of the lift. Even sitting down less during the day can help. But be kind to yourself. If you’re not feeling up to it, don’t put pressure on yourself.
Being active can improve mental wellbeing and quality of life, as well as reducing fatigue. Being active may also have positive effects on your condition , such as reducing the risk of a flare-up. Scientists believe regular exercise could help reduce inflammation in Colitis. This has been seen in other long-term illnesses, but more research is needed to know for sure.
Find out more in our information on being active with Crohn’s or Colitis.
It’s a good idea to talk to your IBD team when you’re planning a pregnancy. They will talk through the importance of keeping well and making sure your Colitis is controlled. They’ll also consider your general health. They’ll review your medicines to check you have the safest possible combination for pregnancy.
Colitis is unlikely to affect fertility if your condition is controlled and you’re feeling well.
If you’ve had pouch surgery, such as restorative proctocolectomy or IPAA, you may have more difficulty getting pregnant. It’s thought that surgery in your tummy could cause scarring around the fallopian tubes and ovaries. This may cause fertility problems. However, there may be less risk with newer surgical techniques, such as keyhole surgery, known as laparoscopy.
No commonly used medicines for Colitis are known to reduce fertility in people with female reproductive organs. However, there are some medicines that may affect your chances of conceiving if you have male reproductive organs:
Find out more in our information on reproductive health.
Speak to your IBD team if you’re planning to get pregnant or if you find out you’re pregnant. You shouldn’t stop taking your medicines unless your IBD team say it’s ok to do so.
Most people with Colitis will have normal pregnancies, births, and healthy babies.
A flare-up in pregnancy increases the risk of giving birth early or having a baby with a low birth weight. Your IBD team should be able to help you to control your condition. With very few exceptions, you can continue most treatments while you’re pregnant.
People with Colitis are more likely to have a caesarean section, known as a C-section, than people who do not have Colitis. However, most people with Colitis can give birth vaginally.
Talk to your IBD consultant and your specialist doctor in pregnancy and childbirth, known as an obstetrician, about your options. A C-section may be recommended if you’ve had pouch surgery.
Find out more in our information on pregnancy and birth and postnatal care and breastfeeding.
Most people who have Crohn's or Colitis in their family will not develop either condition. But your risk is higher if a close family member is affected. Research has shown:
Colitis can occur at any age. Nearly 1 in 5 people have told us that they were diagnosed with Crohn’s or Colitis before the age of 18.
Symptoms are similar to those in adults. Many of the medicines used for adults can also be used to treat children. Some children respond well to medicine and their condition rarely bothers them. Others may need long-term medicines or surgery.
Most children with Crohn’s or Colitis continue to go to school and take part in sports and other interests. They can go on to further education, work, have a family of their own and enjoy life.
For more, read our information on supporting your child with Crohn’s or Colitis.
It is estimated that about 3 in every 10 people with Crohn’s or Colitis are over 60 years old.
Medicines and surgery are treatment options for Colitis in older people. However, there are some extra things your IBD team will consider when recommending treatment options to you.
Many older people have other health conditions, such as high blood pressure or diabetes, and may be taking other medicines. Your body also changes as you age. Your doctor will consider any other illnesses you have when thinking about the best treatment options for you.
Your doctor will look at potential side effects and interactions with other medicines you take. Talk to your IBD team about the risks and benefits of each treatment. You can decide together which is the best option for you.
There is no single definition of disability in use in the UK. Disability Rights UK explain the different definitions. Currently, there is no national register of people who are classed as disabled. But you may be able to register with your local council if you meet their criteria.
A survey we conducted in 2019 found that more than 1 in every 3 people with Crohn’s or Colitis considered themselves to be disabled. If your condition affects your daily life, you may be entitled to help with your finances and protection at work. Some people with Colitis might be able to get a Blue Badge if they get certain benefits or find it hard to walk from their car to where they’re going. Find out more about Blue Badge parking in our information on travel.
The Equality Act 2010 defines when someone is considered to be disabled and is protected from being treated unfairly. Although Colitis isn’t automatically classed as a disability under the Equality Act, it is a condition that might be classed as a disability depending on the effect on your daily life. You may not personally see yourself as being ‘disabled’ but be considered disabled under the legal definition in the Equality Act.
If your employer knows about your Colitis, they can make changes to your workplace to help you do your job. These are called reasonable adjustments. Find out more in our guides for employees and employers.
Living with a long-term health condition like Colitis can have an impact on your financial situation. Our finances information outlines the help and support that may be available.
You could also be entitled to benefits to help you support yourself and your family. Which disability benefit you can apply for will depend on your age and where you live. Find out more in our disability benefits quick guide.
Our helpline team provides up-to-date, evidence-based information. You can find out more on our helpline web page. Our team can support you to live well with Crohn’s or Colitis.
Our Helpline team can help by:
You can call the Helpline on 0300 222 5700. You can also visit our livechat service. Lines are open 9am to 5pm, Monday to Friday, except English bank holidays.
You can email helpline@crohnsandcolitis.org.uk at any time. The Helpline will aim to respond to your email within three working days.
Our helpline also offers a language interpretation service, which allows us to speak to callers in their preferred language.
You can find support from others in the Crohn’s and Colitis community through our virtual social events. There may also be a Local Network in your area offering in-person social events. Visit our Crohn’s & Colitis UK in your area webpage to find out what is available.
This closed-group Facebook community is for anyone affected by Crohn’s or Colitis. You can share your experiences and receive support from others. Find out more about the Crohn’s & Colitis UK Forum.
There are many benefits to becoming a member of Crohn’s & Colitis UK. One of these is a free RADAR key to unlock accessible toilets. Another is a Can’t Wait Card. This card shows that you have a medical condition. It will help when you are out and need urgent access to the toilet. See our membership webpage for more information. Or you can call the Membership Team on 01727 734465.
We follow strict processes to make sure our information is based on up-to-date evidence and is easy to understand. We produce it with patients, medical advisers and other professionals. It is not intended to replace advice from your own healthcare professional.
We hope that you’ve found this information helpful. Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishops Square, Hatfield, Herts, AL10 9NE. Or you can contact us through the Helpline on 0300 222 5700.
We do not endorse any products mentioned in our information.
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
