Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last full review: December 2023
Next review date: December 2026
Crohn’s and Colitis are lifelong conditions that cause inflammation and ulcers in the gut. The symptoms can include:
Getting a diagnosis of Crohn's or Colitis is not always easy. You may need several tests, examinations and investigations. For some people, waiting times can be long. And you may be dealing with embarrassing and distressing symptoms and the anxiety they may bring while you wait.
But you’re not alone. This information is designed to guide you through the process of getting a diagnosis. We hope our information will make things seem less overwhelming, but if you have any questions, then our helpline is here to help you.
Below you can find out about:
This information might use words you have not heard before. Our page on medical words can help provide an explanation.

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Some people may find it embarrassing to talk about their symptoms or may be worried about what the diagnosis may be. But the sooner you find out why you’re unwell, the quicker you can start treatment to help you feel better.
Some important things to remember about Crohn’s and Colitis:
Our symptom checker can help you find out when to talk to your GP and what symptoms to talk to them about. Always talk to your GP if you’re concerned about your symptoms.
I always knew something wasn’t right. It’s not normal to bleed or feel like that. Initially, I felt scared and didn’t want to tell anyone – but being diagnosed helped me come to terms with it and get on with life.
Arizona
Living with Indeterminate Colitis
Make an appointment with your GP if you think you may have Crohn’s or Colitis. If you need urgent medical advice, call 111 or in an emergency, call 999. You can find out more about Crohn’s Disease, Ulcerative Colitis or Microscopic colitis on our information pages.
During your GP appointment they will ask you about:
Tell your GP if you're waking up in the night with pain or urgency to poo. Not everyone experiences this, but telling your GP about night symptoms can help them decide which investigations you need.
Some people find it difficult or embarrassing to talk about poo. Try to remember that talking about these symptoms is an everyday part of a GP’s job. Their focus is to make sure you get the healthcare you need. You can use our appointment guide to help you talk about your symptoms.
It can sometimes be difficult to get an appointment with your GP. Each GP surgery has its way of managing appointments, but if you’re struggling, we have some things you can try:
If you’re employed, you may need to take time off work for a GP appointment. Check if your GP surgery is open at weekends or evenings or try and book an appointment first or last thing in the day. Your employer isn’t legally required to give you time off for medical appointments. Check the policy at your workplace. You may need to take holiday, make up the missed time, or take unpaid leave. You don’t have to tell your employer why you need to see the GP unless you want to.
If you can’t get an appointment with your GP:
Once you have a GP appointment, it’s important to tell them how your symptoms affect you. But it’s not always easy to do this under pressure. Here are some tips to help you:
Read our Appointments guide for more tips about talking to your GP or getting the most out of medical appointments.
Your GP should recommend you have some investigations if you’ve been having any of the following symptoms for more than 6 weeks:
If you have these symptoms, you should speak to a health care professional as soon as possible. Your GP may use the following guidelines to plan which tests you will need and when:
Taking care of your mental health is just as important as taking care of your physical health. But living with symptoms that you may find embarrassing or distressing can trigger lots of different feelings and emotions. You may feel anxious, frustrated, scared, or angry. Not knowing what might happen in the future may make some people feel helpless and uncertain. It’s natural that you may struggle to cope sometimes. In fact, almost half of all people with Crohn’s or Colitis say it’s affected their mental health.
We have lots of honest but reassuring information for you to read, or you can speak to someone from our helpline for support. You can find out more about how others feel and the support that’s available to you on our mental health and wellbeing page.
If you have thoughts of suicide or harming yourself, tell someone you trust, or call the NHS on 111.
If your life is in danger call 999 or go to your nearest A&E.
If you’re feeling emotionally vulnerable, the Samaritans are available to call 24 hours a day, 7 days a week on 116 123.
You can’t be diagnosed with Crohn’s or Colitis from just one test. Your doctor will need to gather lots of information to find out why you’re unwell. This can sometimes take time but it’s important you get the right diagnosis. The symptoms of Crohn’s and Colitis may be like other conditions, such as irritable bowel syndrome (IBS). To help understand what’s going on in your body, your GP will consider all your symptoms, together with some early investigations. These might include an examination of your tummy, as well as tests on your blood and poo. Your GP may also send you to have endoscopies, scans or X-rays. These are all tests to look inside your body.
Your GP might examine your tummy (abdomen) area to check for any lumps or to see if it’s tender. They may also check your bottom for piles, also known as haemorrhoids. You can request a doctor who’s the same sex as you, or you can ask for a chaperone for your examination. A chaperone is someone who can go with you to your examination and is usually the same sex as you, is impartial and does not know you.
Blood tests can show several different things. They can be used to see if you have inflammation in your body. They can also show if you’re low in iron, known as anaemia, or if you lack certain vitamins. Anaemia could suggest that you’re not absorbing the right nutrients or that you have small amounts of bleeding somewhere in your gut. These are both common in Crohn’s and Colitis. Your GP can also order a special blood test to check for signs of Coeliac disease. Coeliac disease is an immune condition that becomes worse when you eat foods that contain gluten. The symptoms of Coeliac disease can be like the symptoms of Crohn’s and Colitis. You can take Coeliac UK's online assessment to see if you should be tested for the condition.
Tell the doctor or nurse before your test if you’re worried about needles or seeing blood. They can make sure you’re as comfortable as possible and answer any questions you have.
Your poo might be tested for signs of bleeding or inflammation. It may also be checked for infections, like a Clostridium difficile infection, often known as C.Diff. For these tests, also called stool or faecal tests, you’ll need to collect a sample of your poo in a clean, dry screw-top container. Your doctor will give you this container and let you know what to do with it. You can find out more on how to collect and store a poo sample on the NHS website.
The thought of needing to give a sample of poo can be off-putting. But these sorts of tests are incredibly useful. They can help with your diagnosis, which means that you get the right sort of treatment for you.
Your GP may arrange for your poo to be tested for something called faecal calprotectin. Faecal calprotectin tests can show if there’s inflammation in your gut. This can be a sign that you may have Crohn’s or Colitis. However, a high faecal calprotectin result can also be caused by other issues, such as diarrhoea from an infection, gastroenteritis or certain types of cancerous and non-cancerous tumours.
Usually, levels that are above 100ug/g (micrograms of calprotectin per gram of poo) are considered to be a raised level. Higher levels may suggest that you should have further tests for Crohn's or Colitis. Not all hospitals and clinics use the same cut-off point of 100ug/g.
Lower levels of faecal calprotectin could indicate that you have irritable bowel syndrome or another non-inflammatory condition. However, lower levels can’t completely rule out Crohn’s or Colitis. You may have a repeat test after 6 weeks if your symptoms carry on.
A faecal calprotectin test may not be helpful for diagnosing Microscopic Colitis. For this condition, faecal calprotectin levels are often quite low.
Just like adults, faecal calprotectin tests are sometimes used to help diagnose Crohn’s or Colitis in children and young people aged under 18. See above for more information.
A child’s calprotectin levels may be assessed by a specialist in a hospital or clinic, rather than a GP.
There are no agreed cut-off levels that reliably show inflammation in children. Sometimes, the same faecal calprotectin cut-off levels as an adult might be used in children over four. But these will be used cautiously.
Children’s levels of calprotectin may be naturally higher than an adult’s and can vary. This can make it difficult to interpret, particularly in children younger than six.
To help with diagnosis, these tests may be used alongside a list of the child’s symptoms. Using both can help give a full picture of what’s going on.
Generally, if you’re older than 60, your GP may not use the faecal calprotectin test. This is because they may want to rule out other conditions, such as bowel cancer. Some hospitals and clinics may not use the faecal calprotectin test for some people with certain symptoms under 60 years old.
Your GP might use a FIT or faecal immunochemical test instead. This can check for small amounts of blood in your poo. Blood in the poo does not always mean a person has cancer. A FIT test may show blood in your poo due to something else, such as Crohn’s or Colitis.
For years I was misdiagnosed with skin conditions and allergies – it only was after finally getting a faecal calprotectin test that I was diagnosed with Colitis. One year later, I'm in remission and getting on with my life.
Megan
Living with Colitis
If your blood and poo tests show inflammation, your GP should refer you to a specialist gastroenterology doctor in an IBD (Inflammatory Bowel Disease) service. They have expert knowledge of gut conditions, like Crohn’s and Colitis, and can do specialist tests. If you have been referred through the NHS e-Referral Service, you may be able to choose which hospital you go to.
It may take some time to get an appointment with your gastroenterology team. The Inflammatory Bowel Disease Standards state that you should have a specialist assessment within four weeks of being referred, but it may take longer.
In a survey, we found that more than 1 in 4 people living with Crohn’s or Colitis waited more than a year to be diagnosed. Waiting a long time for a diagnosis can be difficult, especially as your symptoms may worry you and may impact your daily life. Not knowing how long you will have to wait for an appointment may be frustrating, so it’s important you know what to expect and when.
How long you wait may depend on where you live. Your GP should let you know how long you can expect to wait. Contact your GP surgery if you haven’t heard from the hospital within that timeframe and they can follow up for you. Your referral letter may also have a telephone number for the department you have been referred to. You could also try contacting the hospital’s Patient Advice and Liaison Service (PALS) directly to ask about waiting times.
Tell your GP if your symptoms get worse while you’re waiting for an appointment. If you need urgent medical advice, call 111 or in an emergency, call 999. You can use our appointment guide to help you explain how your symptoms are impacting your quality of life. Your GP may be able to contact the consultant on your behalf to ask if there is any medicine you can take or if you need to be seen sooner.
We have information on managing many of the common Crohn’s and Colitis symptoms. While our symptoms information has been written for people with a diagnosis of Crohn’s or Colitis, you might still find some of the suggestions helpful.
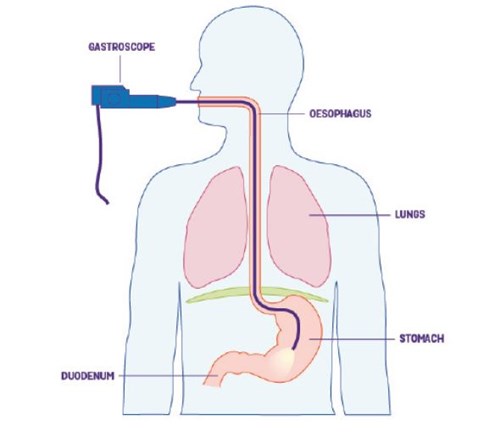
Crohn’s and Colitis cause ulcers and swelling in your gut. To look for these signs, a doctor or specialist may insert a small camera into your mouth or bottom. This type of camera is on the end of a long, thin tube and is called an endoscope. The procedure is called an endoscopy.
An endoscopy is not normally painful, but it might be uncomfortable. To help you relax, you might be offered a sedative. Having any sort of procedure can sometimes make you nervous or anxious, especially if you don’t know what to expect. Your healthcare professional will be able to answer any questions you have. You may also find it reassuring to look at our Facebook forum where people share their stories and experiences.
The risks and benefits of an endoscopy should be explained to you before you give consent (permission) to having the procedure. You can find out more about these procedures and any risks on our tests and investigations page.
During an endoscopy, small samples of tissue are often taken from the gut, known as biopsies. These samples can be looked at under a microscope to help understand what’s causing your symptoms. These tissues samples are essential for diagnosing Microscopic Colitis. In Microscopic Colitis, an endoscopy may not show any visible signs of inflammation. Instead, changes in the gut can only be seen under a microscope. Microscopic Colitis is a type of Inflammatory Bowel Disease that’s different from Crohn’s or Ulcerative Colitis.
Symptoms of Crohn’s and Colitis can come and go. Your symptoms might get better while you are waiting for your appointment. It is still worth having your endoscopy. Your doctor might find signs of inflammation even when you do not have symptoms.
There are several types of endoscopy. The type of endoscopy you have will depend on the part of your gut that needs to be looked at. The main types are:
An endoscope is passed into your mouth to look at the upper part of your digestive system. This includes your throat, stomach and small bowel, also known as the duodenum. You may have this type of endoscopy if you have indigestion or vomiting. It’s not usually used if Colitis is suspected.
An endoscope is inserted into your bottom to look at your large bowel, including your rectum and colon. For a colonoscopy, your colon must be empty of poo. You will need to fast and be given a strong laxative to take around 24 hours before.
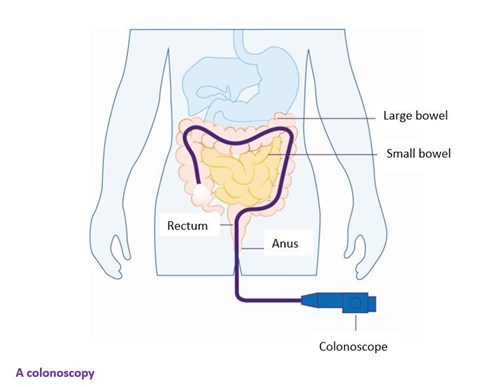
This is like a colonoscopy but only examines the rectum and lower part of the colon. Usually, a flexible endoscope is used, which is bendy and helps the specialist see further up the bowel. You will not need to fast for this procedure. A gentle laxative will be used before the procedure.
Please visit our tests and investigations page to find out about other types of investigations you may have, how to prepare for an endoscopy and if there are any risks.
After your endoscopy, you should receive a report within three weeks. Contact your GP if you haven’t heard back. In some cases, you may be given your report right away, and an endoscopy nurse may explain the results to you. You may be referred for an appointment with a gastroenterologist to talk about your results in more detail.
Some people may feel anxious while waiting for their results. Some people find it helpful to find out more information while they wait, while others prefer the distraction of their normal life. There is no right way to feel, but if you need to talk then contact our helpline for support.
You might need to have another endoscopy in case something was missed the first time. This can happen if the bowel preparation did not fully clear out your bowel before the procedure.
The results on your endoscopy report might not specifically say ‘Crohn’s Disease’ or ‘Ulcerative Colitis’. There are different forms of Crohn’s and Colitis, and their different names suggest where you’re most affected.
Forms of Ulcerative Colitis include:
Forms of Crohn’s Disease include:
Find out more about the forms of Crohn’s and Ulcerative colitis, including information and images of where in the gut you may be affected.
Microscopic Colitis is an Inflammatory Bowel Disease that affects the large bowel (colon and rectum). There are two main forms of Microscopic Colitis – Lymphocytic Colitis and Collagenous Colitis. These are very similar conditions and are commonly referred to under the single name ‘Microscopic Colitis'.
It can be hard to tell whether a person has Crohn’s or Colitis, especially in children. If this happens, you may be given a diagnosis of Inflammatory Bowel Disease Unclassified (IBDU) or ‘Indeterminate Colitis’. Your health care professional will help you find a treatment that works best for you.
The term ‘colitis’ by itself is a general term that means inflammation in the colon. If your endoscopy finds inflammation but no ulcers, your inflamed colon may be caused by something other than Ulcerative Colitis. You may see terms like ‘nonspecific colitis’ or ‘ischemic colitis’ on your endoscopy report. These are not types of Inflammatory Bowel Diseases and are different to Ulcerative Colitis. Your healthcare professional will help you understand more about these conditions and will be able to support you further with these conditions.
After diagnosis, the Inflammatory Bowel Disease Standards state that you should:
Your GP should be informed of your new diagnosis and the care plan that has been agreed within 48 hours.
Finding out you have Crohn’s or Colitis can be a shock. But now that you can put a name to your symptoms, you can start to manage them. And we’re here to help, every step of the way. We’ve helped thousands of people access the information they need to find answers. We can help you get support and take control.
Read our newly diagnosed information to find out more about:
You can also find out more about Crohn’s and Colitis, including possible symptoms, treatments and living with these conditions.
Don’t get too overwhelmed. When I was diagnosed, I panicked. It felt like my world was falling apart. So, I’d tell myself not to spend time worrying about what may or may not happen. Instead, listen to the doctors, read up on it yourself, and know that you will find a point where it all feels normal. It’ll become so day-to-day that you won’t even think about it.
James
Living with Colitis
Have you recently been diagnosed with Crohn’s Disease, Ulcerative Colitis or Microscopic Colitis?
Our eight, bite-sized, weekly emails can help you:
Sign up to our new series of emails to help you navigate life after diagnosis.
If your endoscopy didn’t find anything, you could still have Crohn’s or Colitis. You may need more tests and investigations, such as an X-ray, ultrasound or MRI scan to check for inflammation. Find out more in our Tests and investigations information.
Microscopic Colitis, a type of Inflammatory Bowel Disease, can sometimes be difficult to diagnose. If you have Microscopic Colitis, then your colon and rectum may look normal on a colonoscopy. During a colonoscopy, a tissue sample, known as a biopsy, may be taken from your gut. This biopsy will be looked at under a microscope for signs of Microscopic Colitis, which is the only way to diagnose it. You may have to wait a few weeks after your endoscopy to get the results of the biopsy back.
If further tests still can’t explain your symptoms, you might have another condition. Your healthcare professional will tell you about the next steps.
We know it can be frustrating not to have a clear answer to what’s making you feel unwell. It can sometimes take a bit of time to reach the correct diagnosis. You may find it helpful to keep a record of the symptoms you experience so you can show your doctor.
It’s important to raise your concerns with your healthcare professional if you think your diagnosis is incorrect.
Here are some things you can do if you have doubts about your diagnosis.
If you’ve asked for a second opinion, your GP may be able to make a recommendation of who to see. Some people may want to do their own research to find a particular hospital or specialist to be referred to. Due to funding restrictions, your GP may not be able to refer you to your chosen specialist. Your GP does not have to refer you if they think you do not need a specialist assessment or specialist treatment. You can find how your local hospital is performing compared to the IBD standards on the IBDUK website.
Each of us has the right to good healthcare. We also have the right to complain if we don’t think we’ve received this. You may want to make a complaint if:
If appropriate, you might be able to deal with the issue straight away by raising your concerns informally. You could talk to your healthcare professional directly and let them know what’s wrong. If you’re not comfortable doing this, you could speak to someone who isn’t directly involved.
This should be within 12 months of the incident or you becoming aware of it. You can make a complaint in writing, by email or verbally. If you’ve made a verbal complaint, make sure you write down everything you’ve discussed. You should also be provided with a written copy of what was said by your NHS service.
When making any complaint, keep a record of any communication that takes place.
If you’re complaining on behalf of someone else, make sure you provide their written consent. If that person can’t give their consent, for example, if they’re a child, lack mental capacity or have died, you may be able to make a complaint on their behalf.
When making a complaint, include:
All NHS services are required to have a complaints procedure. You may be able to find this on your GP website or you could speak to a receptionist about how to make a complaint. You should make your complaint as soon as possible.
If you want to raise an issue about something within a hospital, you could speak to the hospital Patient Advice and Liaison Service (PALS). This is a service that most hospitals have and is free, confidential and independent.
You can find out more about to make a complaint below:
Health professionals can order some publications in bulk by using our online ordering system. If you would like a printed copy of any of our information, please contact our helpline.
Our helpline is a confidential service providing information and support to anyone affected by Crohn's or Colitis. Our team can:
Email helpline@crohnsandcolitis.org.uk
This closed-group community on Facebook is for everyone affected by Crohn's or Colitis. You can share your experiences and receive support from others.
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn's or Colitis. All events are open to members of Crohn’s & Colitis UK.
We follow strict processes to make sure our information is based on up-to-date evidence and easy to understand.
Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishop Square, Hatfield, AL10 9NE, or contact us through our Helpline: 0300 222 5700
Understanding Crohn's and Colitis
Read information
Living with Crohn's or Colitis
Read information
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
