Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last updated: December 2024
Last full review: October 2024
Next review date: October 2027
You may not have heard of Microscopic Colitis before. It’s a type of Inflammatory Bowel Disease, or IBD. Microscopic Colitis affects the colon, causing symptoms such as ongoing, watery poo and tummy pain and cramps.
Being told you have Microscopic Colitis can be a shock. You might be feeling anxious about what comes next and how your life might change. But you’re not alone.
Now that you’ve put a name to your symptoms, you can start to manage them. And we’re here to help, every step of the way.
This information is for anyone who has Microscopic Colitis, thinks they might have it or wants to learn more about it. It looks at:

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Microscopic Colitis is a type of Inflammatory Bowel Disease. When you have Microscopic Colitis your immune system does not work properly, causing inflammation. This can lead to frequent, watery diarrhoea that keeps coming back. It can also cause tummy pain, fatigue and bloating.
Microscopic Colitis is a lifelong condition. But the right treatment can make a huge difference to your quality of life. This can help you get your condition under control, and there will be times when you have fewer symptoms or none at all. But you may also experience relapses, when your symptoms return or get worse.
As information about the condition increases, it is becoming better known and understood. More cases are being diagnosed as our understanding develops.
Microscopic Colitis affects the colon, which forms part of the large bowel. Normally, your colon absorbs water from digested food, which helps you pass a solid, soft and well-formed poo. But when the colon is affected by Microscopic Colitis, it cannot absorb as much liquid. This can mean that fluid builds up, producing a large amount of watery diarrhoea.
The walls of your colon have layers. In Microscopic Colitis, the inner lining becomes inflamed. This inflammation can only be seen when a sample of tissue, known as a biopsy, is taken from your colon and looked at under a microscope.
There are two main types of Microscopic Colitis:
These two main types of Microscopic Colitis look different under the microscope. But the symptoms and treatment are the same.
Sometimes, a biopsy sample may not look healthy but a diagnosis of LC or CC cannot be made. This may be because the number of white blood cells is not high enough and the inner lining may not be thick enough. If this happens, you may be given a diagnosis of Microscopic Colitis incomplete, also known as MCi.
Have you recently been diagnosed with Crohn’s Disease, Ulcerative Colitis or Microscopic Colitis?
Our eight, bite-sized, weekly emails can help you:
Sign up to our new series of emails to help you navigate life after diagnosis.
Microscopic Colitis has not been known about for as long as Crohn’s or Ulcerative Colitis.
Crohn’s can affect any part of your gut, from your mouth to your bottom. Ulcerative Colitis only affects your large bowel, which includes the colon and rectum. Microscopic Colitis only affects the colon.
With Ulcerative Colitis, doctors may use a camera on a long flexible tube, called an endoscope, to look at the lining of the large bowel. The doctor will be able to see the inflammation on the lining of the large bowel. But with Microscopic Colitis, your colon will usually look healthy when looked at through a endoscope. The doctor will need to take samples, called biopsies, of the colon and look at them under a microscope to see the inflammation that Microscopic Colitis causes.
Microscopic Colitis carries less risk of serious complications than Ulcerative Colitis or Crohn's. But it is a serious condition that can have a huge effect on quality of life.
The main symptom of Microscopic Colitis is ongoing watery diarrhoea. Diarrhoea is the passing of watery or loose poo more than three times a day for longer than four weeks. For some people, this can be as many as 15 times during the day and night. It can begin suddenly or gradually, and can get worse over time.
With Microscopic Colitis, the diarrhoea:
When you have diarrhoea, your body loses a lot of fluid. It is important to drink plenty of fluids to avoid getting dehydrated. Find out more in our information about diarrhoea and dehydration.
Other symptoms can include:
My symptoms include explosive diarrhoea, stomach cramps and tiredness. I have also lost a lot of weight.
Lyn
Living with Microscopic Colitis
These symptoms can have a huge impact on everyday life. They can make it difficult to work, go out with friends or plan activities.
You may find our information on symptoms helpful. It includes information on diarrhoea, fatigue, bloating and wind, and joint pain. Most of the evidence for this information is based on studies of Crohn’s and Ulcerative Colitis. This is because there is not as much research available on Microscopic Colitis.
Coping with these symptoms may have an impact on your mental health. Coping with a long-term condition like Microscopic Colitis can be difficult and some people may feel isolated and low. But there is support available. Find out more in our information on mental health and wellbeing.
Nobody told me some of the things I might experience, like fatigue or joint aches.
Helen
Living with Microscopic Colitis
We do not know what causes Microscopic Colitis. It may be caused by different factors.
These factors include:
Microscopic Colitis can affect anyone, from any background, age, ethnicity or sex. But there are some risk factors that may mean you are more likely to get it. These factors include:
Around 1 in every 2,000 people are thought to have Microscopic Colitis in the UK. But the real number could be a lot higher. This is because the condition may be underreported and misdiagnosed.
Microscopic Colitis has been linked to some other autoimmune conditions. An autoimmune condition is caused by the immune system attacking other parts of the body.
Around 4 in 10 people with Microscopic Colitis also have an autoimmune condition.
These may include:
Having these conditions makes it more likely that you will have Microscopic Colitis as well.
Another autoimmune condition closely associated with Microscopic Colitis is coeliac disease. This is a condition that causes your immune system to attack your gut when you eat gluten. Gluten is a type of protein found in wheat, barley and rye.
Both conditions affect the production of white blood cells and have similar symptoms. These can include diarrhoea, bloating and tummy pain. This means Microscopic Colitis can sometimes be misdiagnosed as coeliac disease.
You can have both conditions together. You are more likely to have Microscopic Colitis if you already have coeliac disease. If you do have both, you may still have diarrhoea on a gluten-free diet if your Microscopic Colitis is not treated.
IBS is a common, lifelong condition affecting the digestive system. Many of its symptoms are very similar to the symptoms of Microscopic Colitis. These include diarrhoea, tummy pain and bloating. The exact cause of IBS is not known, and there is no cure. But medicines and careful changes to diet can usually help keep the symptoms under control.
Microscopic Colitis is sometimes misdiagnosed as IBS. This is because their symptoms are so similar, and IBS is more well known in comparison. Some people may have both conditions at the same time. Around 1 in 10 people with IBS involving diarrhoea may also have Microscopic Colitis. This can make diagnosis difficult. This means that sometimes people do not receive the correct diagnosis and treatment as quickly as they should.
Some evidence suggests that Microscopic Colitis may sometimes develop into Crohn’s or Ulcerative Colitis. At the moment, we do not understand how this happens, but the risk of this happening is small.
Around 4 out of 10 people with Microscopic Colitis also have BAM. This is when bile acids used in digestion cannot be reabsorbed as usual and cause bile acid diarrhoea (BAD).
BAM is treated with bile acid binders. These medicines work by binding to the bile acids in your gut. This stops them from reaching the colon so that they cannot cause diarrhoea. You may be offered bile acid binders if your Microscopic Colitis is related to BAM. You may also be offered bile acid binders if other treatments do not stop your diarrhoea.
If your healthcare professional thinks your Microscopic Colitis is related to BAM, you may be sent for a special test called a SeHCAT scan.
There is more on SeHCAT scans in the section how is it diagnosed? Find out more about BAM in other treatments. Find out more about diarrhoea, including how to manage it, in our information on diarrhoea.
Microscopic Colitis does not make you any more likely to get colon cancer than the general population.
Talk to your GP if you think your symptoms could be caused by Microscopic Colitis. Your GP will need to take a history of all your symptoms. This may help them rule out other conditions.
Poo tests, known as faecal calprotectin tests, are often used to help diagnose Crohn’s and Colitis. This test may not be useful for Microscopic Colitis. In Microscopic Colitis, calprotectin levels are often normal or only slightly raised.
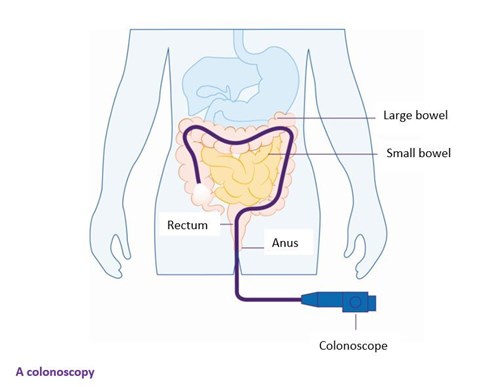
If your GP thinks you may have Microscopic Colitis, you will need to be referred for a colonoscopy and a biopsy. You may also need to be tested for other autoimmune conditions, such as coeliac disease.
It may take time to diagnose Microscopic Colitis. This is because the condition is not always as well-recognised as other forms of Inflammatory Bowel Disease.
See our appointment guide for information on getting the most out of your appointments. This includes tips about talking to your healthcare professional.
In Microscopic Colitis, signs of inflammation can only be seen under a microscope. You will need to have a colonoscopy so that a tissue sample, or biopsy, can be taken.
During a colonoscopy, a long flexible tube is inserted through your bottom. The tube is about the thickness of your little finger, with a bright light and camera at its tip, This lets the doctor look at the lining of your colon. During the procedure, a biopsy is taken from your colon. This is then looked at under a microscope.
Most colonoscopies are performed under mild sedation. This is when you are given medicine through a tube in your arm to make you feel relaxed. You may be offered gas and air or painkillers instead, to make you more comfortable.
You can find out more in tests and investigations, or read more about colonoscopies on the NHS website.
I was diagnosed by a biopsy taken during a colonoscopy. This followed 6 months of unexplained weight loss, persistent frequent diarrhoea and abdominal pain.
Michaela
Living with Microscopic Colitis
You will be given a small capsule of synthetic bile salts to swallow. This contains a small amount of harmless radioactive material known as SeHCAT. You will then have a scan, followed by another one a week later. These will measure how the bile salts have been absorbed.
See our information on tests and investigations for more on SeHCAT scans. And there is more on bile acid malabsorption in our information on diarrhoea.
It may take time to get a diagnosis of Microscopic Colitis, which can be frustrating.
This may be because:
If it is taking a long time to get diagnosed, you may find our information on how to get a diagnosis useful.
You may also find it helpful to keep a symptom diary, which you can take to healthcare appointments. When you have a symptom, try recording the date and time with a short description of what happened. Give the symptom a rating from ‘mild’ to ‘very severe’. Try to add any details that might be helpful, such as any food or medication that may have had an impact. These could help your healthcare professional rule out other conditions.
Many people find it uncomfortable to talk about diarrhoea and difficult to share how concerned they are. It can be upsetting to feel like you are not being listened to by your healthcare professional. Being able to self-advocate, or speak up for yourself, can be useful in making sure your voice is heard. You may find the information on self-advocacy in our appointment guide helpful. It includes tips on communicating your symptoms and talking to your healthcare professional.
It's been hard to get a diagnosis and treatment. Even after that Microscopic Colitis is still not considered to be as serious as other conditions.
Lyn
Living with Microscopic Colitis
There are several changes to your lifestyle that may improve your symptoms. Your healthcare professional may suggest:
Before offering any treatment for Microscopic Colitis, your doctor will check if you take any medicines for other conditions.
Medicines that may make your Microscopic Colitis symptoms worse include:
Many of these medicines can also cause diarrhoea as a side effect. You can read more about some of these medicines in our information on other treatments.
Making changes to your lifestyle may help to reduce your symptoms.
Many people ask:
Talk to your doctor or dietitian before making any major changes to your diet. They can help you plan how to avoid certain foods while still getting the nutrients you need.
After many years of experimenting, I have found dairy products seem to trigger my symptoms, so I have replaced milk with soya or almond milk instead.
Lyn
Living with Collagenous Colitis
If you smoke, stopping can help. Smoking increases the risk of Microscopic Colitis. People who smoke have symptoms that are worse and less likely to get better with treatment. Your GP practice can offer support with stopping smoking.
There may be several options for treatment depending on the severity of your symptoms. These include:
If you have mild Microscopic Colitis, medicines to stop diarrhoea, such as loperamide, can help. These make food move through the gut more slowly and allows more water to be absorbed. Poo becomes firmer and you may need to go to the toilet less urgently. They can also help to control symptoms while other medicines take time to work. Find out more in our information on diarrhoea.
Bile acid binders, such as colestyramine or colesevelam, attach to the bile acids in your gut. You may be offered this medicine if your Microscopic Colitis is related to bile acid malabsorption (BAM). It may also be offered if you continue to have diarrhoea despite other treatment. Find out more in our information on other treatments.
Budesonide is used to reduce inflammation to control symptoms of Microscopic Colitis. This steroid has been found to help some people who have moderate to severe Microscopic Colitis. As with all steroids this is not usually a long-term option. Find out more in our information on steroids.
Azathioprine and mercaptopurine may help some people if budesonide has not worked. Find out more in azathioprine and mercaptopurine.
It’s rare to need surgery if you have Microscopic Colitis. Your healthcare professional may suggest surgery if other treatments have not worked. You can find out more about possible operations in surgery for Ulcerative Colitis.
Our Helpline takes many calls from people with Microscopic Colitis, so you are not alone. We cannot advise but it may help to talk through your worries. Your doctor will support you and you should ask for support from an IBD nurse-led service.
An IBD nurse can offer support and advice about treatment options and daily life with Microscopic Colitis, and help you to live well with IBD. But NHS support services vary – unfortunately some hospital IBD teams do not treat Microscopic Colitis. And some areas still do not have an IBD nurse, while others have limited resources and may not be able to support you if you have Microscopic Colitis.
Find out if your hospital has an IBD nurse.
Our Helpline team can provide information and support to anyone affected by Inflammatory Bowel Disease. You can find more information, including contact details, below and on the Helpline webpage.
We’re here for you whenever you need us. Our award-winning information covers a wide range of topics. From treatment options to symptoms, relationship concerns to employment issues, our information can help you manage your condition. We’ll help you find answers, access support and take control.
All information is available on our website at crohnsandcolitis.org.uk/information.
Our Helpline team provides up-to-date, evidence-based information. They can support you to live well with Crohn’s or Colitis.
Our Helpline team can help by:
You can call the Helpline on 0300 222 5700. You can also visit crohnsandcolitis.org.uk/livechat for our LiveChat service. Lines are open 9am to 5pm, Monday to Friday, except English bank holidays.
You can email helpline@crohnsandcolitis.org.uk at any time. The Helpline will aim to respond to your email within three working days.
This closed-group Facebook community is for anyone affected by Crohn’s or Colitis. You can share your experiences and receive support from others at facebook.com/groups/CCUKforum.
There are many benefits to becoming a member of Crohn’s & Colitis UK. One of these is a free RADAR key to unlock accessible toilets. Another is a Can’t Wait Card. This card shows that you have a medical condition. It will help when you are out and need urgent access to the toilet. See crohnsandcolitis.org.uk/membership for more information. Or you can call the Membership Team on 01727 734465.
We follow strict processes to make sure our information is based on up-to-date evidence and is easy to understand. We produce it with patients, medical advisers and other professionals. It is not intended to replace advice from your own healthcare professional.
We hope that you’ve found this information helpful. Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishops Square, Hatfield, Herts, AL10 9NE. Or you can contact us through the Helpline on 0300 222 5700.
We do not endorse any products mentioned in our information.
Living with Crohn's or Colitis
Read information
Living with Crohn's or Colitis
Read information
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
