Everyone says it… ‘Please, take a seat!’
Rachael
Living with Crohn's
From being in meetings to taking public transport, this is generally recognised as a kind offer. But, for many years taking a seat was one of the worst suggestions anyone could have made to me! While living with Crohn’s or Colitis can take its toll, developing a fistula due to my Crohn’s added another element to my battle.
Fistulas can affect both men and women and although not everyone with Crohn’s or Colitis develops fistulas, I did. A rectovaginal fistula is an abnormal connection between the rectum and the vagina. Fistulas can allow wind and faecal matter to pass through the vagina and cause infections, soreness, discharge, and abscesses.
The physical pain and discomfort of this aside, my fistulas also had a mental and emotional impact.
This can lead to depression, anxiety, social inhibitions and the loss of intimacy with a partner. I certainly felt a loss of femininity.
In 2014 my health began to deteriorate rapidly. I experienced lethargy, weight loss, pain, bleeding, and discharge from both the anal and vaginal areas, which were the first signs and symptoms of the developing fistulas. These were quickly followed by constant infections and abscesses and I couldn’t control the leaking faecal matter or wind.
Looking back, my Crohn’s had started many years before.
These were the symptoms that led to my official diagnosis of Crohn’s Disease. Until then, I had been told I had Irritable Bowel Syndrome (IBS) and had to “learn to live with it.”
While trying to keep clean became a 24-hour battle, the mental and emotional effects of the fistulas were having a huge impact upon my confidence and self-esteem. Over time, I had five setons inserted to help drainage over the course of my treatment. These are commonly used in an attempt to heal the fistulas and prevent infections, but I found setons themselves to be painful to live with.
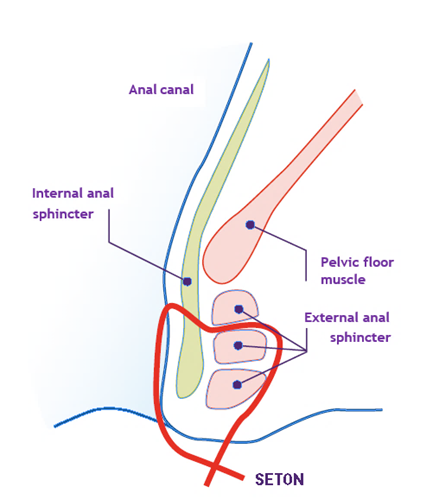
Setons
Loose setons are soft surgical threads. The surgeon passes these through the opening in the skin, along the track of the fistula and out through the anus. It’s then tied to form a loop. The ends hang out of your anus, allowing the pus or infected tissue to drain away. The seton is usually left in for several weeks and removed if the fistula is healing. Studies show that adding loose setons to infliximab treatment leads to better results for people with anal fistulas. Some people say that a loose seton feels like having a rubber band hanging out of your bottom, but after a few days they no longer notice it’s there. In some cases, setons are used as a long term treatment if fistula healing is unlikely.
Loose seton
It is quite embarrassing to tell someone that I have a little rubber band coming out of my bum (a seton). But I only tell people I trust and feel comfortable with, and they have been really supportive.
Finlay, age 23
Living with Crohn's
At this point I also had a loop ileostomy formed and commenced infliximab and azathioprine in an attempt to calm down my Crohn’s and heal my fistulas. While this helped, I would still have bouts of vomiting, abdominal pain, and further rectovaginal infections.
The loop ileostomy was turned into an end ileostomy with stoma bag and I underwent more surgery including a Martius graft. This meant taking fatty tissue from around the labia majora, opening up the perineum and then grafting the tissue (with its ready blood supply) around the area of the fistula.
Early post-op signs were good but, ultimately, the graft failed and I was devastated.
Both physically and mentally the fistulas continued to have a huge impact and I decided enough was enough. Living with a stoma and on constant rounds of antibiotics and anti-inflammatory suppositories, my symptoms were still increasing in intensity. I have two brilliant consultants and they, along with my IBD team, had thrown everything they had at these fiendish fistulas. While they were obviously as frustrated as I was, we finally agreed to go ahead with a proctectomy and permanent colostomy.
It’s now just over 12 months since I had that surgery and it was the best decision I’ve ever made. Don’t get me wrong, permanently living with a stoma has its issues, but living with active fistulas, seton drains and constant infections was no longer an option for me.
Living with Crohn’s and a fistula doesn’t just affect a person’s physical health but their mental and emotional health too.
While I did share some information with a few trusted friends and family members, they were never fully aware of my struggle. Rectovaginal fistulas can be terribly embarrassing and because of this good information, empathy and support are scant.
I battled on, learnt a lot, and made some life-changing decisions. Speaking out and sharing my experience in the hope that it may help others (both people living with fistulas and health care professionals) is one of those decisions.
Education, encouragement, and empathy are the keys to overcoming the aspects of this disease that I found demoralising and debilitating.
At the age of 51 I’d begun studying for a PhD. When the fistulas came along, I thought my studies would never come to fruition. Yet, with a good dose of dogged determination and support I did complete my research and in 2018 I gained my doctorate. I was so proud and I felt worthwhile again.
Now, whenever someone says ‘please, take a seat,’ I smile to myself! Don’t get me wrong, sitting for long periods can still be uncomfortable, but that’s because of scar tissue, and that is something I can definitely live with!

