Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Health appointments can be daunting when you have Crohn’s or Colitis – no matter how many you’ve attended before.
There’s a lot to think about.
But you’re not on your own.
This information will help you get the most out of your time with health professionals, and focus on what matters to you. Download My appointments journal (PDF) to help you take note of how you’re feeling in between appointments, and keep everything neatly in one place. You may find it easier just to download and print the appointment pages (PDF).
Let us know your experiences using My appointments journal - email us at evidence@crohnsandcolitis.org.uk for the chance to share your experiences with the Crohn's and Colitis community.
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Not everyone’s IBD team looks the same - but whoever you see, they’re all working to help keep you as healthy as they can.
Here are some of the health professionals and how can they help:
Remember that there may be another health professional who can help you reach a specific goal. You could ask if there’s anyone who can support you with diet or nutrition, looking after your mental health or alternative approaches to living with the condition.
If you want to, you can ask for a second opinion. Use our interactive map to search for local hospitals who have specialist services for IBD.
We've helped create guidelines on what quality care should look like at every point of a patient’s journey – from first symptoms, to diagnosis, treatment, and ongoing care. These are the IBD Standards.
Keep a note of your team:
Your triggers
It can be helpful to note down things that trigger symptoms for you. Maybe it’s stress, certain foods - making notes will help you understand more about what you should (if you can!) avoid.
What helps you in a flare?
Make a note of tried and tested ways you can feel better. Have a plan of action that you’ve developed with your doctor or IBD nurse around what to do in a flare. Does your IBD service have a flare card? See our information for tips on what to do if you're having a flare.
Your goals
Your health professionals probably won’t know what your priorities are. So setting goals for what you want out of your treatment is really useful for staying focused.
What’s your normal?
Let your health professional know what‘s usual for you - it’s easy to get used to living with symptoms that you shouldn’t.
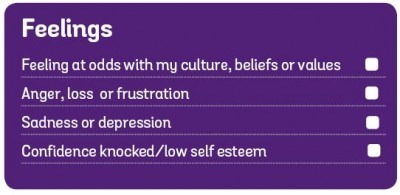
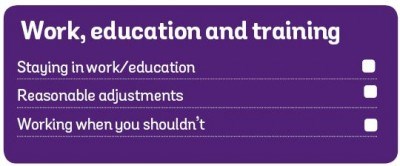
Crohn’s and Colitis affect more than just guts. Think about what's bothering you and let your health professionals know.
My consultant asked me for a goal and I said it was to stand in a field with no toilets around. For a long time toilets were like a security blanket - I always had to know where the nearest one was.
So, the idea of going to Peru and doing the Inca trail - it felt like an impossible journey. But that’s where we’ve just gone on holiday. I’m not worried at all now
Paul
Living with Ulcerative Colitis



Can you help me understand...?
So, you mean...
...and repeat back what you’ve understood.
Ask health professional to draw a diagram to help show things like:
It takes guts to be assertive with your doctor. But being clear about your needs is the best way to get the most out of your time, so don’t be afraid to ask questions about what matters to you.
Your feelings and symptoms are valid. Health professionals see a variety of people, some of whom are very ill. But don’t let what you’re going through be dismissed. Needing the toilet five times a day may seem less serious in comparison to others, but it doesn’t mean it’s not having a huge impact on your life.
Don't worry about looking bad - if you've been really busy, forgotten to take your medicine, haven't been tracking your symptoms, or cancelled your dietician appointment, make sure you're open about it.
Jaya
Living with Ulcerative Colitis
There’s no right or wrong way to say how you feel, or describe symptoms. Here are some words and phrases that might be helpful along with some handy tools.
Don’t be afraid to use emotive language to say how bad things are for you.
I’m worried about...
I can’t…
I’m struggling to...
I’m not coping with...
My quality of life has got worse
I’m not happy with how my treatment is going
Fatigue
Describing your poo
Not sure what to ask at your appointment? Not to worry - we’ve put together a useful list of questions that people with Crohn’s or Colitis often want to know.
Pick the ones that are most relevant to you. You don’t need to ask everything at once – if you think of something later, you could send an email or call. We have a wealth of information about Crohn's and Colitis which can also help answer general questions.
Make a list of questions, make a list of symptoms and frequency and take pictures if needed!
Tom
Living with Crohn's
Keep notes so you're prepared. You can use the pages in My appointments journal (PDF).

Before you leave your appointment, check that you know what will happen next. These questions can help clear up any uncertainty.
Keep a note of how it went, what your health professional has agreed to do and what you've agreed to. My appointment journal can help with this.
If you'll soon be transitioning from paediatric to adult care for your Crohn's or Colitis, our Transition guide has all the information you need to help you to understand what might happen and how you can prepare for appointments with your new team.
Have you used My appointments journal at an appointment for your Crohn's or Colitis? We'd love to hear how it went! Email us at evidence@crohnsandcolitis.org.uk and we may share your experience online.
Crohn’s & Colitis UK received funding from Pfizer and AbbVie, who had no input into the content or design of this information.
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Signposting you to specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
